SAN FRANCISCO - The term "fixed dosimetry" may be a misnomer in that patients actually receive a wide range of radiation dose during intravascular brachytherapy, according to a presentation Wednesday at the American Society for Therapeutic Radiology and Oncology (ASTRO) meeting.
Specifically, a multi-institutional group looked at 3-D treatment planning and dose-volume histogram (DVH) analysis to assess the actual radiation dose delivered when fixed dosimetry methods are employed. The researchers also performed Monte Carlo simulations and radiochromic film measurements of an 192iridium multiple seed train (Best Medical International, Springfield, VA) in order to demonstrate the high doses delivered by 192Ir electrons between seeds.
"We as radiation oncologists should give radiation therapy with the same rigor, the same exactitude, and the same level of confidence that we have when we treat cancer [traditionally]. Because if radiation therapy matters, then it matters how you give it and how you assess it," said Dr. Louis Harrison, who headed up the team. Harrison is the director of Continuum Cancer Centers of New York, the co-director of the Institute for Head and Neck Cancer, and chairman of radiation oncology, Beth Israel Medical Center and St. Luke's-Roosevelt Hospital Center, all in New York City.
The intravascular ultrasound (IVUS) results and angiographic measurements from 20 cases in the Washington Radiation for In-Stent Restenosis Trial (WRIST) were used for this study. The fixed dosimetry levels for WRIST were 15 Gy at 2 mm from the source for vessels smaller than 4 mm in diameter, and 15 Gy at 2 mm for larger vessels.
"The treatment approach, which is very straightforward, is to dose the target area and protect the normal organs within a very tight range," Harrison said. "The entire target is covered by a minimum dose. This allows us to assure ourselves that we’ve given proper treatment to the target and minimized the risk of injury to the normal tissue."
The adventitial tissue layers (the target area) and the intimal tissue layers (normal tissue) were contoured using volumetric IVUS. DVHs, and their associated parameters, ranging from D90 to D1, were calculated at these layers.
Angiograpic review provided longitudinal source placement information. The DVH was calculated at the stent edges. Finally, centering issues were examined with the assumption that the seeds were centered on the IVUS tip and that the seeds were localized in the geographic center of the lumen.
Monte Carlo simulations were performed for a 5-seed train, with less than 5% standard deviation reached for energies scored within 1 mm of the interseed air gap axis. GafChromic film measurements were performed for an 192Ir 6-seed train to verify the dose distributions at radial distance of 0.5 mm to > 2 mm.
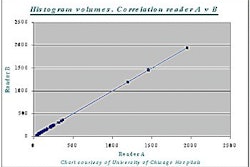
"If you’ve got a situation where 20 patients have gotten the same dose, these dose volume histograms should be superimposed. But what we have here is almost 20 different lines suggesting that each of the 20 patients had completely different dosimetry, despite the fact that they were each given the same dose," Harrison said.
According to the results, the actual doses received to the adventitia and intima were heterogeneous, with the majority of patients not receiving the prescribed dose of 15 Gy. The average DVH values and radiation dosages were as follows:
Intima
- Dv90, 12 Gy
- Dv50, 19 Gy
- Dv10, 34 Gy
- Dv1, 58 Gy
Adventitia
- Dv90, 7 Gy
- Dv50, 11 Gy
- Dv10, 16 Gy
- Dv1, 23 Gy
"As you get to smaller volumes of intima, we are giving substantially larger doses of radiation than most of us would have realized," Harrison pointed out.
Monte Carlo and radiochromic film results showed that high doses were deposited by 192Ir elections between seeds for a multiple seed train. At very close distances, the electron dose exceeds the dose from 192Ir gammas. The total dose near the interseed air gap can be 160 Gy delivered at 0.5 mm and 58 Gy at 0.8 mm.
"Fixed dosimetry prescriptions result in a large heterogeneous dose, and make it impossible to assure oneself of the dose to the target area to any individual or population of patient," Harrison said.
In order to accurately gauge the efficacy of radiation therapy, a method must be devised for predicting the dose to the adventitia so that the exposure to the intima is kept at a minimum, he added.
"Fixed dosimetry prescriptions, while they seem expedient to cardiologists and others in the cath lab, are a very heterogeneous treatment with a potentially heterogeneous outcome," Harrison said. "We need a better understanding of DVH 3-D treatment planning and analysis to allow a better understanding of dosimetry and efficacy. [Not] until we do that will we really know what we’re doing with coronary artery radiation therapy."
By Shalmali PalAuntMinnie.com staff writer
November 8, 2001
Copyright © 2001 AuntMinnie.com