Accelerated partial-breast irradiation (APBI) combines high radiation doses, and a shorter treatment period, with one of four delivery methods including interstitial brachytherapy or intraoperative radiation therapy. While enthusiasm for APBI continues to grow, little is known about the delayed tissue toxicity associated with this technique, according to a study in the International Journal of Radiation Oncology, Biology, Physics.
"This study is the first to provide some specific dosimetric parameters to guide clinicians in defining, at least with respect to late tissue effects, what constitutes an optimal interstitial HDR (high-dose-rate) implant," wrote Dr. David Wazer and his fellow radiation oncologists from Tufts-New England Medical Center in Boston, Rhode Island Hospital in Providence, and the Medical College of Virginia in Richmond (IJROPB, February 2006, Vol. 64:2, pp. 489-495).
For this six-year study, 75 patients with early-stage breast cancer from the Virginia and Boston institutions were enrolled. Eligibility criteria were extensive and included unicentric primary cancer with invasive ductal histology. Excision was repeated until gross tumor removal was achieved in all patients. Chemotherapy was given at the discretion of the consulting oncologist and, if used, initiated two to six weeks after APBI.
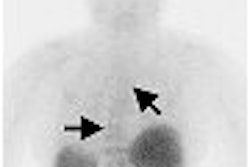
All patients were treated with an iridium-192 HDR interstitial implant with a source strength of 3-10 Ci. Implants were placed either perioperatively or within eight weeks of definitive breast surgery.
"The planning target volume (PTV) was defined as that volume encompassed by the excision cavity plus a 2-cm margin of breast tissue.... A dose of 3,400 cGy in 10 fractions was prescribed as the minimum dose anywhere with the prescription volume," the authors explained. Postimplant CT was performed for dosimetry.
"To minimize skin doze, the source was kept a minimum of 5-7 mm from the skin surface at the ends of each catheter," they wrote.
Patients were followed up with mammography at six months and one year after implantation and then annually. They were assessed using a previously published global cosmetic score (Journal of Clinical Oncology, March 1992, Vol. 10:3, pp. 356-363).
The median follow-up time was 73 months with no patient experiencing greater than grade 1 skin toxicity, the authors stated in their results. The majority of women rated the cosmetic outcome as excellent (67%). Grade 0 or 1 toxicity was found in 96% of the patients.
The total volume of implanted breast tissue correlated with cosmetic outcome, and the number of dwell positions was significantly associated with a suboptimal cosmetic score, the authors stated.
In addition, dose hot spots (V150 and V200) and the dose homogeneity of the implanted volume (DHI) were also associated with higher-grade skin toxicity. Dose hot spots also were associated with an elevated risk for fat necrosis.
Finally, the authors found that chemotherapy was linked to increased risks for fat necrosis, higher-grade skin toxicity, and suboptimal cosmetic score. They recommended that clinicians "proceed with caution" when prescribing chemotherapy after APBI.
Wazer's group highlighted the following take-home points from their study:
- Keep volume as low as possible while maintaining coverage of PTV.
- Minimize hot spots.
- Maintain a high level of global dose uniformity as defined by DHI.
- Interpret short-term follow-up results conservatively as tissue effects can vary with time.
By Shalmali Pal
AuntMinnie.com staff writer
February 13, 2006
Related Reading
Permanent seed implants reduce radiotherapy burden in breast cancer, January 5, 2006
Breast MR helps refine partial-breast irradiation, October 19, 2005
Copyright © 2006 AuntMinnie.com