Radiation therapy is an effective treatment for patients with early-stage breast cancer, but at what risk of developing other cancers? Findings from studies presented at last month's European Society for Therapeutic Radiology and Oncology (ESTRO) annual meeting document there is higher risk to these patients.
Results of two studies conducted in Denmark and France were discussed at ESTRO's London conference. Collectively, they represented the long-term outcomes of almost 64,000 women.
In the French study, Dr. Alain Fourquet, chief of the department of radiotherapy of the Institut Curie in Paris, presented data about the risk of developing second malignancies in a cohort of 17,745 women who received treatment at the facility between 1981 and 2000. Approximately 82%, or 14,512 women, received radiotherapy treatment, and 18%, or 3,233, did not. Approximately 7,000 additional patients were not included in the analysis, including all male patients, women who had a prior history of cancer or had metastatic cancer, and women who had been diagnosed with bilateral breast cancer.
Radiotherapy delivery included cobalt-60 linear accelerators that were in use during the earlier years of the study data. The types of adjuvant chemotherapy treatments administered to some of the patients varied over time.
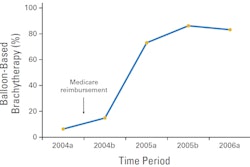
The 15-year overall survival rate was 70% for all patients, who were followed from two to 29 years, Fourquet said. A total of 2,370 women, or 13.4%, developed a second malignancy at a median follow-up of 13.4 years, with a slightly higher percentage in the group who received radiotherapy treatment (13.8%) compared with11.1% in the group who did not.
13.4-year risk of breast cancer patients developing a second malignancy
|
In comparison with the general population of women in France, the breast cancer patients had a statistically significant increased risk of developing second malignancies at a standardized incidence rate (SIR) of 2.96. The greatest risk increases were seen in hematological malignancies (SIR: 2.4), lung cancers (SIR: 1.39), and gynecological cancers (SIR: 1.31). None of these cancers was related to radiotherapy treatments, Fourquet said.
However, the breast cancer patients had lower incidences of gastrointestinal and head and neck cancers than the general population. Rates of malignant, melanoma, genitourinary, and thyroid cancers were comparable.
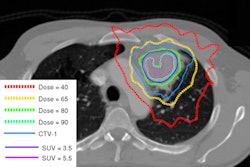
Regarding the impact of different treatments on the risk of second malignancies, the study identified an increased incidence of sarcoma and lung cancer with radiotherapy, as well as an increased risk of colorectal cancer and leukemia with chemotherapy. "The cumulative incidence at 15 years following treatment was 0.49 for sarcoma, and 0.8 for lung cancer, with an increased rate of risk in the long term," Fourquet reported.
Danish study
The Danish study included 46,176 women and evaluated the long-term risk of developing a second primary cancer. It revealed that women who received radiotherapy treatment had an increased risk of developing several second primary cancers located in or close to the treatment field. Trine Grantzau, a doctoral candidate at the department of experimental clinical oncology at Aarhus University Hospital, also advised ESTRO attendees that she and her colleagues determined that the risk increased over time.
Data from the Danish Breast Cancer Cooperative Group, linked to the Danish Cancer Registry, were analyzed for women treated for early breast cancer between 1982 and 2008. Fifty-one percent, or 23,627 women, received postoperative radiotherapy treatments; 49%, or 22,549 women, were not irradiated.
"From 1997 onward, it was found that the number of women treated with postoperative radiotherapy has increased. This is probably due to women treated with breast-conserving operations and the introduction of breast screening in Denmark," Grantzau said.
By the end of 2008, at a median follow-up of six years, the total patient cohort had developed 2,595 second primary cancers. Of these, 44% were at sites exposed to radiotherapy at doses that were potentially carcinogenic, Grantzau said.
"At 15 or more years after treatment, the risk of a second primary cancer increased to 1.9 in the irradiated women compared to 1.1 in the nonirradiated women. For women who had sites classified as radiotherapy-exposed, we found a SIR of 2.1 for irradiated versus 1.3 for nonirradiated women. Sites not exposed to radiotherapy showed no increased risk," she added.
Regarding lung cancer, the hazard ratio was found to increase significantly over time, to 3.5 for irradiated patients 20 years after treatment. Grantzau found a SIR of 4.3 among irradiated patients versus 0.7 in nonirradiated patients. A similar pattern was seen for esophageal cancer.
In the discussion period, Dr. Klaus Trott from the department of radiation oncology of St. Bartholomew's Hospital in London addressed the issue of the price for cancer cure.
"Is the risk of radiotherapy-induced cancer the price for cure versus pain? Second cancers are only one of the unwanted effects for consideration against local recurrence and death from uncontrolled cancer. This has to be compiled into one balancing act, which asks: 'Is this a price worth paying? Is the risk and the price the same for every patient?' The answer is no," he emphasized.
The risk of second cancer varies with local dose, technique, patient anatomy, and age at radiotherapy, and more data are needed, Trott concluded.
"To reduce risk, we require knowledge of dose and anatomical dose distribution. This only comes from case-controlled studies. They are urgently needed," he said.