Radiation therapy (RT) following a radical prostatectomy can improve biochemical progression-free and survival outcomes for high-risk prostate cancer patients, yet fewer than 20% receive the treatment. A decision analysis study published online June 9 in the Annals of Oncology makes a strong case for its utilization.
In 2010, prostate cancer treatment in the U.S., including both includes both initial and supplemental costs, reached approximately $12 billion, according to estimates from the U.S. National Cancer Institute (NCI). Approximately 20% of patients who undergo a radical prostatectomy have a recurrence, and the rate increases to 40% to 60% for those with adverse pathological features.
Is it clinically better and more cost-effective to treat a high-risk patient with adjuvant radiotherapy immediately following surgery, or should regular prostate-specific antigen (PSA) tests be performed and salvage radiotherapy initiated only if a patient's PSA levels rise? Researchers at Thomas Jefferson University Hospital decided to find out.
Dr. Timothy Showalter, a radiation oncologist at the hospital's Bodine Center for Cancer Treatment, and colleagues developed a decision analytic model to estimate the cost of adjunct radiotherapy compared to observation only.
The group analyzed data from participants in the Southwest Oncology Group (SWOG) 8794 clinical trial, a randomized study of treatment versus observation patient outcomes. Of the 431 patients enrolled, 242 had a pretreatment PSA level of ≤ 0.2 ng/mL and a positive surgical margin, seminal vesicle invasion, and/or extracapsular extension.
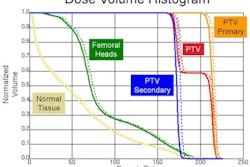
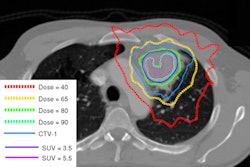
The research team's objective was to determine the cost per PSA success when adjuvant radiation therapy was used compared to observation, based on the conditions and outcomes of the SWOG 8794 trial. All costs were based on the published national average for 2010 Medicare reimbursement rates. The researchers assumed that four-field conformal radiotherapy was delivered to 60 to 64 Gy.
Patients who underwent radiation therapy had a higher PSA success rate than those in the observation group over a 10-year period. The cost for this treatment was $15,900, compared with $9,876 for observation only. However, if the authors had estimated the cost of intensity-modulated radiation therapy (IMRT), the cost would increase by an additional $10,000, they noted.
The decision analysis did not assess quality-of-life gains.