A treatment combining tumor cyst drainage with fractionated stereotactic radiosurgery (SRS) seemed to be safe and effective for adult craniopharyngioma patients at Tokyo Medical University Hospital, according to an article published in the International Journal of Radiation Oncology, Biology, Physics.
Craniopharyngiomas are a type of brain tumor derived from pituitary gland embryonic tissue. The tumor is typically a large single cyst or multiple cysts, most commonly located near the hypothalamus. The majority of patients (approximately 60%) are adults 50 to 60 years old; the remainder are younger than 16 years.
Treatment of these brain tumors, which are rare and usually slow-growing, is mired in debate. Left alone, they can impair vision and cause endocrinologic dysfunction. However, treatment options, whether surgery, radiation therapy, or both, can cause serious lifelong morbidities.
No consensus exists on the best course of treatment to avoid hypothalamic injury and to prevent recurrence. Total resection is recommended when a tumor is favorably located, but when it involves hypothalamic or optic structures, limited surgical excision followed by local irradiation is recommended. With either type of surgery, there is a risk of damaging the pituitary gland and/or the hypothalamus. Because of the need to keep radiation dose to normal tissues low, radiation therapy is also challenging.
Lead author Dr. Naoto Kanesaka, PhD, of the hospital's departments of radiology and neurosurgery, and colleagues initiated a treatment strategy combining cyst aspiration with fractionated stereotactic radiosurgery. After reducing the volume of the tumor through cyst drainage, fractionated SRS delivered high radiation doses to the tumor and reduced doses to the surrounding normal tissue (Int J Radiat Oncol Biol Phys, June 28, 2011).
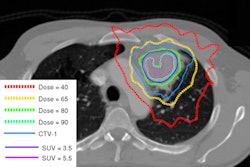
A total of 16 patients, ranging in age from 22 to 74 years, underwent this treatment between 1999 and 2005. Median tumor volume reduction by cystic drainage through the transcranial root using endoscopy was 68%, with a range of 33% to 90%. For most patients, tumor shapes were irregular after cyst aspiration.
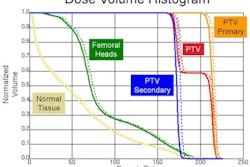
To treat these irregularly shaped tumors, several foci were irradiated. Radiation therapy treatment planning was performed to cover the planned target volume within the 80% dose line of the prescribed doses. Patients received 30 Gy of radiation in six fractions over a 12-day course of treatment. The dose to the optic nerve did not exceed 24 Gy.
All patients were followed through November 2009, with a median follow-up period of 52 months. The three-year local control rate was 82.4%. Six patients had a complete response, eight had a partial response, one did not respond to treatment, and one progressed. Three of the patients experienced recurrence, including the patient whose tumor progressed. Based on this response to treatment, the authors wrote that they would prescribe increased radiation doses of fractionated SRS for future patients.
None of the patients has died as a result of the tumor, although one patient died of thyroid cancer (the thyroid was not exposed to radiation during the treatment). Two of the three patients who had tumor recurrence underwent surgery, and the third patient had a second course of fractionated SRS.
"We believe that fractionated SRS is better than single-fraction SRS when critical organs, such as the optic nerve, are adjacent to the tumor," the authors wrote.
While hormonal functions did not improve in any patient, half of the patients had improved vision approximately 2.5 months after treatment. The authors attributed this to the reduced tumor volumes, and the fact that the radiation therapy did not damage the optic nerve.