How long can the economies of European countries afford to provide radiotherapy treatments to a steadily increasing percentage of their populations diagnosed with cancer?
This question is not addressed in an article in press published 26 August in Radiotherapy and Oncology comparing the cost of radiotherapy at a Belgian hospital in calendar years 2000 and 2009. However, the content of the article -- a financial cost model showing how expenses almost doubled during the course of a decade of cancer treatment technology evolution -- brings this issue to the front of a reader's mind.
In Belgium, the 88.8 million euro ($126 million U.S.) budget to provide radiotherapy services in 2009 was twice the amount budgeted in 2000, an increase explained in part by a 40% surge in the number of patients who needed treatment, according to the article's corresponding author Dr. Yolande Lievens, a radiation oncologist at the University Hospitals Gasthuisberg in Leuven, Belgium.
And at University Hospitals Leuven specifically:
- The cost of capital investments by the department of radiation oncology increased by 96% in 2009 compared with 2000.
- Personnel costs in the radiotherapy department increased by 103%.
- The cost of resources to provide electron-beam radiotherapy treatments (EBRT) increased by 89%, from an expenditure of 4.5 million euros ($6.4 million) in 2000 to 8.6 million euros ($12.2 million) in 2009.
- The number of EBRT treatment-related activities also skyrocketed, more than doubling from a total of 2.7 million activities in 2000 to 5.5 million activities in 2009.
The cost allocation model
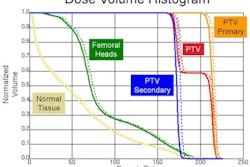
In 2000, the hospital developed a detailed cost model for its department of radiation oncology. It was updated in 2009 to incorporate and capture new types of costs incurred by new types of treatment, such as stereotactic body radiotherapy (SBRT), volumetric arc radiotherapy, image-guided radiotherapy, respiratory-gated radiotherapy (RGRT), and intensity-modulated radiotherapy (IMRT).
The model is based on ABC costing methodology, which assumes that activities consume resources to produce products. The model includes resource costs and activities costs.
Resource cost categories include hospital overhead costs to support the department; costs associated with the physical space and rooms of the radiation oncology department; wages for clinical, administrative, and support staff; costs of equipment acquisition and maintenance; and material costs (both consumable products and reusable products, such as a stereotactic frame).
Activity costs are categorized as being treatment-related, department-supported, and hospital-supported. Products are defined as the list of irradiation treatments that the department offers to patients. All costs are ultimately allocated to products.
The cost model verified what the authors presumed: Costs increase with treatment complexity, and more quality assurance activities also are needed to guarantee safety as complexity escalates. The authors cited the example of 3D conformal radiation therapy (CRT), which resulted in cost increases of approximately 30% for tangential breast and high-grade palliative treatments. Because the number of fractions for a treatment directly impacted costs, increased use of hypofractionated schedules would decrease costs of a particular treatment, and helped offset other costs incurred by its increased treatment complexity.
2000 vs. 2009
The authors used EBRT, a treatment that was performed throughout the decade, to evaluate cost changes and trends. The most significant activity trend was that the percentage of cost allocated to quality assurance increased by 13%, from 10% in 2000 to 23% of the total in 2009. The percentage of cost of portal imaging, which had just begun to be used in 2000, increased from 2% to 14% of the total EBRT cost in 2009. However, overall treatment delivery costs, which included these two categories, remained relatively stable, at 69% and 73% in 2000 and 2009, respectively.
The department became more efficient over the decade with respect to both planning treatments for patients and daily radiotherapy treatment delivery. These costs declined respectively from 31% to 27% and from 56% to 45% of the total.
Resource costs allocated to EBRT also were very consistent during the decade. All costs were adjusted to the value of the euro in 2009.
|
"Whether governments remain able and willing to cover cost increases largely depends on the economical and political climate, both determining the accepted growth in healthcare budgets," Lievens and colleagues noted. While they believed the improved quality of current radiotherapy technology would ultimately improve patient outcomes, increased investment in radiotherapy treatments required solid evidence on the added medical effectiveness of new interventions combined with accurate data on their extra cost, they added.
ESTRO's HERO project
The European Society for Radiotherapy and Oncology (ESTRO) concurs. It has initiated an ambitious Health Economics in Radiation Oncology (HERO) project to develop a knowledge base and a model for health economic evaluation of radiation oncology in Europe. The project will address the need for radiotherapy, provision and accessibility of treatments, waiting lists, staffing, cost accounting, and economic evaluation.
Headed by Lievens and Dr. Cai Grau, a radiation oncologist at the Aarhus University Hospital in Denmark, an 11-member task force of experts from Europe and Canada is in the process of conducting an evidence-based survey of the need for radiotherapy in Europe based on cancer epidemiology within different European countries. The aim is to assess the actual status of radiotherapy in Europe through a Web-based information/documentation center that will include the actual levels of radiation oncology infrastructure, equipment, and staffing in different European countries. It will include data on the actual treatments delivered on an annual basis per country.
The cost accounting software model in development will allow users to calculate cost data at multiple levels: from the European and country level, to a department level, to a product (specific irradiation treatment) level. It will benchmark costs at various levels. Its users will be able to evaluate productivity at the national and department level and estimate the budgetary impact of evolutions in technology. The model will also have the ability to perform sensitivity analyses, such as the costs in cases of evidence-based versus actual radiation oncology practices.
Economic models will also be developed to compute value for the cost of radiotherapy treatments. Users of these models will be able to evaluate and compare the cost-effectiveness and cost-utility of different radiotherapy treatments and techniques, as well as compare radiotherapy treatments with other oncology treatments that could be substituted. Users will be able to analyze various cost expenditures to treat a cancer patient, and project them against data relating to patient outcomes.
Ideally, the data generated by the HERO project will be able to be used for key policymaking decisions. The HERO Task Force hopes to complete its project and present its final results in 2013.