A study published in the April issue of Health Affairs comparing two types of effective radiotherapy treatments for prostate cancer found that intensity-modulated radiation therapy (IMRT), the more expensive of the two, may be overused.
A multidisciplinary team of researchers from the University of Michigan in Ann Arbor suggested that the U.S. economy and healthcare reform initiatives may be better served by paying for treatment that works, even if it does not incorporate the newest, and often most expensive, treatments (Health Affairs, 2012, Vol. 31:4, pp. 750-759).
In the United States, more than 200,000 men are diagnosed with prostate cancer each year. Their treatment costs approximately $7 billion per year and is growing at a rate of 11% per year, according to lead author Dr. Bruce Lee Jacobs, a clinical lecturer in urology.
Concerned that newer, more high-tech, and more expensive radiation therapy treatments might be contributing to the increase in treatment expenses, the researchers decided to compare the utilization of two prostate cancer treatment therapies: 3D conformal radiation therapy and IMRT. They used the Surveillance, Epidemiology, and End Results (SEER) database to evaluate Medicare patients who received either type of treatment between 2001 and 2007.
The study evaluated patient demographics, tumor characteristics, type of treatment, and comorbidities of 36,490 men, as well as the rate of cancer recurrence for a subset of patients who had been followed for at least three years. The patients were categorized as low risk if they had well-differentiated tumors or if they had moderately differentiated tumors and were at least age 65 or older at the time of diagnosis. All other patients were categorized as having high-risk prostate cancer.
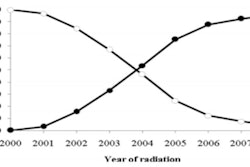
Throughout the entire study period, 54% received IMRT treatment. In 2001, 24% out of 5,275 men underwent IMRT; 45% of this group was categorized as having high-risk prostate cancer compared to 43% in the 3D conformal radiotherapy group.
By 2007, the proportion of patients having IMRT more than tripled to 83% out of 5,421 patients. Seventy-three percent of this group was categorized as high risk, while 82% of the patients who had 3D conformal radiotherapy treatment were high risk.
Reasons for rapid adoption
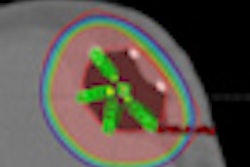
The researchers proposed three reasons for the dramatic increase in adoption and utilization of IMRT. The more conformal and higher dose delivery of IMRT may provide better cancer control and lower morbidity. However, it was the opinion of the authors that evidence for this is mixed.
In their study, they determined that the subset of men followed for at least three years had a lower risk of cancer recurrence if they underwent IMRT treatment (6%) instead of 3D conformal radiotherapy (9%) but that they had a higher risk of having a bowel (22% versus 18%) or urinary (8% versus 6%) complication.
The second reason the authors proposed for the increase in IMRT usage was patient demand for the latest radiotherapy treatment and the pressure that physicians felt to offer it to them despite its elevated expense.
The third reason was financial. Reimbursement by Medicare for IMRT treatment was five times more (approximately $14,000 more) than conventional treatment due to equipment cost, treatment planning required, treatment delivery time, and quality assurance time associated with the procedure.
"Financial pressures induced by considerable start-up costs may encourage IMRT use in the marginal patient," they wrote. For example, the authors referenced marketing materials from Urorad Healthcare of McAllen, TX, which claimed that treating 1.5 new patients monthly with IMRT could generate more than $425,000 in additional annual revenue per physician.
"The concern about overuse of IMRT as a result of high reimbursement rates is compounded by the prospect of physicians' ownership of treatment facilities and self-referral," Jacobs et al wrote, citing a 2006 study estimating that replacing 3D conformal radiotherapy treatment with IMRT for prostate cancer patients alone would increase spending by $1.4 billion per year.
"At issue is what price society is willing to pay for small incremental benefits in outcome from a more costly technology. In the context of limited resources, does everybody deserve a Cadillac when a Buick is almost as good?" they asked.
Their conclusion: Paying for what works will serve the U.S. best in its endeavor to expand healthcare coverage while limiting overall spending.
ASTRO comments
The American Society for Radiation Oncology (ASTRO) issued a statement in which it defended IMRT as a major therapeutic advance for men with prostate cancer. It cited a study using SEER data of prostate cancer patients treated between 2000 and 2009 that showed IMRT treatment improved cancer control, significantly reduced toxicity to the rectum, and reduced hip fractures.
However, ASTRO applauded the University of Michigan research team for addressing the issue of self-referral abuses and physician greed. ASTRO attributed increase in costs to self-referral by urology-owned radiation therapy centers, stating that, "mega-urology practices that can dominate prostate cancer diagnosis and treatment services in their market areas ... likely played a role in the growth of IMRT use during the study period."
ASTRO noted that the Baltimore Sun, the Wall Street Journal, and the Washington Post all have conducted investigations that exposed self-referral abuse in urologists' use of IMRT.
Georgetown University in Washington, DC, is conducting an independent analysis of the effect of physician self-referral on urologists' use of IMRT treatment for prostate cancer patients, a national study underwritten by the society. ASTRO also noted that the U.S. Government Accountability Office (GAO) has been requested by Congress to investigate the clinical and economic impact of physician self-referral on urologists' IMRT use.