Dear AuntMinnie Member,
Is proton therapy worth the cost for treating men with prostate cancer? Maybe not, according to a new study published in the Journal of the American Medical Association.
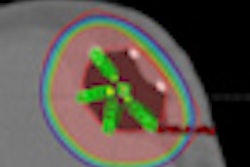
The study compared the effectiveness of three types of radiation therapy treatments for prostate cancer: conventional conformal radiotherapy, intensity-modulated radiation therapy (IMRT), and proton therapy, a relatively new (and incredibly expensive) technology.
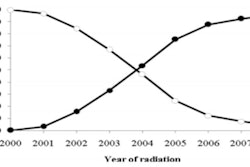
The authors found that IMRT has largely replaced conformal radiation therapy for prostate cancer treatment, and, indeed, there were several advantages to using IMRT in this patient population. But the benefits of proton therapy are less clear, they wrote.
The study is just one strain in a growing chorus that is advising healthcare providers and public policymakers to look more closely at proton therapy before it begins to take hold. Learn more by clicking here.
Also in our Radiation Oncology Digital Community, read about a recent study that looked at outcomes for breast cancer patients treated with a strut-adjusted volume applicator (SAVI) compared to conventional accelerated partial-breast irradiation (APBI). You can find that article by clicking here, or go to radiation.auntminnie.com.
Overdiagnosis and DCIS
In other news, we're featuring several articles from last week's National Conference on Breast Cancer (NCBC) in our Women's Imaging Digital Community.
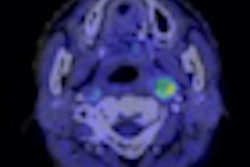
First up is an article that addresses the thorny issue of ductal carcinoma in situ (DCIS). Detection of DCIS has risen sharply since the introduction of breast screening, to the point where some 25% of newly diagnosed cancer is DCIS.
But do these lesions really represent a health threat to women? Or are we "overdiagnosing" by treating them the same as invasive cancer? That's the tantalizing question posed in an article you can reach by clicking here.
In other NCBC news, the world of breast imaging has been buzzing after an advisory panel at the U.S. Food and Drug Administration last week recommended that an automated breast ultrasound (ABUS) system be approved for marketing.
Breast imagers have many other ultrasound tools at their disposal besides ABUS, though, and how to use these tools was the subject of another NCBC presentation. From high-resolution ultrasound to elastography, Dr. Bruno Fornage from MD Anderson Cancer Center walks you through the benefits and drawbacks of each approach.
His advice? Sometimes getting back to basics is the best strategy. Read more by clicking here, or visit the community at women.auntminnie.com.