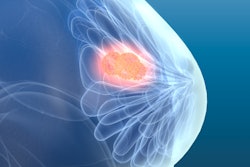
A single dose of targeted radiotherapy during a lumpectomy procedure proved effective in a long-term clinical trial of thousands of women with early-stage breast cancer. The international team behind the large, randomized trial published their results on August 19 in the BMJ.
The trial evaluated up to 19-year outcomes of women treated with targeted intraoperative radiotherapy (TARGIT), a form of radiotherapy delivered directly to the affected area during lumpectomy surgery. Targeted intraoperative radiotherapy is believed to result in lower costs and fewer visits for patients.
The vast majority of TARGIT patients only needed one treatment, and the group had comparable long-term outcomes to those who underwent weeks of conventional whole-breast external-beam radiotherapy (EBRT). The TARGIT group also had lower rates of death from causes other than breast cancer.
"The long-term results of this trial have shown that risk-adapted single-dose TARGIT given during lumpectomy can effectively replace the mandatory use of several weeks of daily postoperative whole-breast radiotherapy in patients with breast cancer undergoing breast conservation," wrote the authors, led by Dr. Jayant Vaidya, PhD, from University College London.
The international team has been studying TARGIT as an alternative to EBRT for years. Their early research found that a single TARGIT treatment was as good as a course of EBRT in controlling cancer, but clinicians have been hesitant to offer patients TARGIT treatment without long-term data.
The new trial continued the team's original stage III clinical trial comparing TARGIT and EBRT outcomes among patients with early-stage breast cancer. From 2000 to 2012, the trial recruited 2,298 patients in 10 countries who had elected to undergo wide local excision instead of mastectomy.
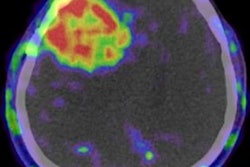
At the outset of the study, patients were randomized into two groups: one to receive conventional EBRT treatment and one to undergo TARGIT therapy. Patients randomized into the TARGIT group underwent 20 to 50 minutes of radiotherapy at the same time as their lumpectomy procedure. The applicator was placed direction in the tumor, sparing skin tissue from radiation.
Eight out of 10 patients in the TARGIT group only required one radiotherapy treatment. Despite the vast majority of patients needing limited radiotherapy, the TARGIT group experienced comparable outcomes to patients with longer radiotherapy treatment courses.
At the five-year mark, 2.11% of TARGIT patients experienced local recurrence compared to 0.95% EBRT patients. This 1.16% difference in five-year local recurrence rate was well below the 2.5% clinical significance threshold set by clinicians and patients at the outset of the trial.
When the authors looked at even longer-term outcomes, TARGIT fared about the same as EBRT. The two treatment methods had no significant differences in survival without local recurrence, invasive local recurrence, mastectomy, distant disease, or breast cancer mortality rates.
Surprisingly, the TARGIT group also had significantly lower mortality rates for causes other than breast cancer (3.95% versus 6.40%). In fact, one analysis showed TARGIT's mortality benefit only grew stronger over time.
The authors didn't know what contributed to the difference in deaths unrelated to breast cancer, but they pointed to prior research showing cardiovascular and lung cancer risks associated with modern radiotherapy treatment.
It's also important to note that some women in the TARGIT group received supplemental EBRT if they met predefined risk factors, including a surgical tumor-free margin less than 1 mm or lymph node positivity.
The research team intends to continue studying TARGIT and have already begun two additional clinical trials. The authors also plan to create a web tool to help physicians use the same risk-managed TARGIT protocol they employed in the study in hopes of providing more patients with the option of TARGIT therapy.
"We believe that the long-term data presented in this paper, together with many benefits for the patient, provide compelling evidence in favor of TARGIT as an effective alternative for this large group of patients with early breast cancer who are suitable for breast conservation," they wrote. "Ultimately the treatment patients receive should be their choice and they should be provided with the data in a format which is transparent, straightforward, and easily understood."