Pseudoaneurysm of the femoral artery is a common result of puncturing the vessel to perform various catheterization procedures such as angioplasty and stent placement. While surgical repair was the traditional method of choice for treating them, ultrasound-guided compression repair gained favor in the early 1990s when it was shown to be effective, and generally safer than surgery.
However, a study published in the May issue of Radiology (Vol. 215:1, pp. 403-408) concludes that US-guided direct thrombin injection is faster, more comfortable, and has a far higher success rate than compression repair of iatrogenic pseudoaneurysms of the femoral arteries.
Drs. Erik Paulson, Douglas Sheafor, Mark Kliewer and others from Duke University Medical Center in Durham, NC, authored a study of 26 patients who underwent US-guided thrombin injection to treat femoral pseudoaneurysms from September 1998 to February 1999. The results were compared with a much larger group of patients who, between January 1992 and September 1998, underwent manual compression therapy, then considered the first line of therapy until the hospital adopted thrombin injection as its treatment of choice in September 1998.
"(Bovine) thrombin is a potent enzyme that transforms fibrinogen to fibrin, the critical component of blood coagulation," the authors wrote, noting that in wide use as a topical agent or as a spray after vascular or cardiac surgery, it has proved to be both safe and effective.
Manual compression repair
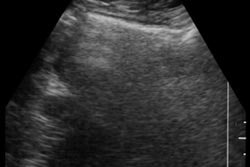
In the 281 patients who underwent compression repair (following the techniques of Fellmeth et al), ultrasound images of the puncture site were obtained in real-time with transducers ranging from 3.5 to 7 MHz, the authors wrote.
The transducer was then oriented to display the pseudoaneurysm neck optimally, and manual compression was applied to the neck for 10-20-minute periods in order to arrest blood flow into the dilated vessel. Compression was released briefly between the periods in order to switch operators or assess the degree of thrombosis achieved. The procedure continued until the blood flow was stopped completely, or until patient or operator fatigue compelled termination, at the discretion of the attending radiologist, the authors wrote. The patients were then told to lie in bed with the affected leg held straight for 4-6 hours. Follow-up color Doppler exams at 24-48 hours were performed only when the procedure was unsuccessful, or in the presence of a compelling clinical indication such as a persistent pulsatile mass or bruit.
Thrombin injection
The 26 patients who underwent thrombin injection (following the techniques of Kang et al) were first scanned with ultrasound using a GE Medical Systems Logiq 700 scanner with a 5-7.5 MHz linear-array or curved linear-array transducer. The researchers studied the anatomy of the pseudoaneurysm, in particular to delineate the relationship of the flow lumen to the underlying pseudoaneurysm neck and artery.
They examined the surrounding soft tissue for evidence of an arteriovenous fistula or multiple interconnecting pseudoaneurysm lobes, and confirmed the patency of the artery and vein. With the aid of a detachable biopsy guide, a 22-gauge spinal needle was inserted into the flow lumen, and a (mean) 350 U of bovine thrombin was injected directly into the flow lumen, the authors wrote. Taking particular care to avoid inadvertent puncture of the pseudoaneurysm neck, the needle was also positioned in the lumen flow away from the neck to reduce the risk of downstream embolization.
Blood flow was monitored with color Doppler US, and a second thrombin injection (100-300 U) was administered in cases where thrombosis was only partial, with or without needle repositioning. Thrombosis usually occurred quickly; the mean time for complete thrombosis was 6 seconds.
As in patients treated with compression, 4-6 hours of bed rest with the affected leg held straight followed the procedure, but these patients underwent color Doppler US follow-up at 24 hours in all cases.
Results and discussion
Thrombin injection brought about complete thrombosis in 96% (25/26) of the patients, significantly higher than the 74% (209/281) success rate for manual compression, the authors wrote, although in six cases some residual blood flow was seen following the procedure, and a small amount of blood was seen in two patients at the 24-hour follow-up. Moreover, there were no complications resulting from the thrombin treatment, foot pulses did not change, and conscious sedation was not required. There were no cases of recurrent pseudoaneurysm at the 24-hour follow-up, they wrote.
While compression repair is considered relatively safe and effective, the authors noted several drawbacks, including pain, difficulty of administration, and the unpredictable duration of the procedure.
"To add a compression procedure to an already overtaxed US schedule is onerous because the procedure occupies an examination room for 1-2 hours and is physically exhausting for both patients and physicians," the authors wrote.
Nevertheless, compression might still be the preferred alternative in a few cases, such as when the pseudoaneurysm has a short, wide neck, which increases the risk of downstream embolization. Both known complications of thrombin injection were due to embolization of the downstream arterial system, the authors wrote.
However, some pseudoaneurysms are not amenable to compression, they wrote. And although it could be argued that compression is a reasonable first step before attempting thrombin injection, compression distorts the pseudoaneurysm anatomy considerably, making it difficult to position the needle accurately in the event thrombin injection becomes necessary later on.
"In summary, we believe that thrombin injection is a superior technique to compression repair," they wrote. "The results of our preliminary work suggest that for most iatrogenic femoral arterial pseudoaneurysms, thrombin injection should replace compression repair as the first line of therapy."
By Eric Barnes
AuntMinnie.com staff writer
May 26, 2000
The full text of the Radiology article can be found at http://radiology.rsnajnls.org/cgi/content/full/215/2/403
Let AuntMinnie.com know what you think about this story.
Copyright © 2000 AuntMinnie.com