
AuntMinnie.com presents the fifth in a series of columns on the practice of ultrasound from Dr. Jason Birnholz, one of the pioneers of this modality.
Fellow UltraSounder,
This special American Institute of Ultrasound in Medicine (AIUM) meeting edition of my column will have two special firsts for AuntMinnie.com readers: a new ultrasound sign and the creation of Web portal where the clinical ultrasound community can collaborate to expand the role of this marvelous form of imaging.
 |
| Dr. Jason Birnholz. |
A graphic case of flushing
I want to introduce the new finding with a case of carcinoid syndrome. The hallmarks of the syndrome are sudden episodes of bright red facial flushing, often associated with abdominal pain, weakness, fainting, and palpitations. Osler described this before 1900 as a puzzling occurrence in "neurasthenic women."
In the 1950s, there was a link found between seemingly random episodes of flushing and a malignant (neuroendocrine) carcinoid tumor arising in the gut that had metastasized to the liver. Flushing (and hypotension) were due to escape of serotonin into the systemic circulation. Carcinoid tumors most often arise in the gastrointestinal tract, but they are found in other locations including the trachea or a bronchus; most are slow growing, benign, and have limited endocrine production.
The case in question is a woman who has had typical and progressively severe carcinoid attacks with florid flushing and a profound decrease in blood pressure for more than 15 years. She has had every imaging test known at a variety of facilities, all directed toward finding the tumor responsible and all uniformly uninformative.
We went over the heart, abdomen, and pelvic viscera with typical transabdominal and endovaginal transducers, and the only thing that could be found that might be related to the carcinoid syndrome was a tiny reflective patch adjacent to the lower pole of the right ovary, which was mildly sensitive to probe pressure. We were intrigued when the patient mentioned that she had to wear very loose clothing, because pressure on some parts of her abdomen would provoke an attack.
She had also learned the hard way that there were other attack triggers, including aspirin, penicillin, and most anesthetic agents. So, we whipped out the 15-MHz array that we love for superficial work and found that abdominal subcutaneous fat was studded with soft, reflective, discrete nodules, a few of which had coalesced into larger collections along the belt line. Minimal pressure on a larger clump elicited facial and upper chest flushing almost immediately.
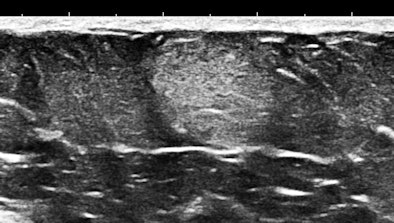
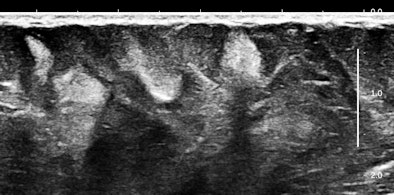
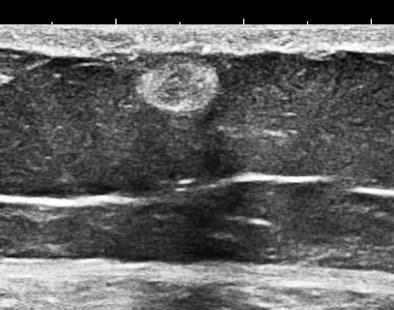
Here are three representative (HD) anterior abdominal wall images at 15 MHz:
 |
| All images courtesy of Dr. Jason Birnholz. |
 |
 |
Mast cells and mediator-release disorders
These echogenic "nodules" are tumorlike collections and cellular infiltrates of mast cells. The precise diagnosis is systemic mast cell disease. Symptoms are due to mediator release. At one pole is typical carcinoid syndrome involving serotonin and kallekrein, and at the other extreme is anaphylaxis with predominant histaminelike substances. Because of the large number of nodules, there is a significant neuroendocrine burden, similar to the multiple metastases of a malignant carcinoid tumor filling the liver.
Fortunately, there are drugs that can block mediator release from mast cells, and there are as yet unexplored possibilities for destroying these nodules percutaneously, which would be similar in concept to debulking a solid tumor as part of the treatment plan.
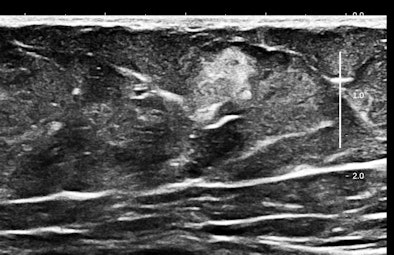
Of course, any of you might say that systemic mastocytosis is such a rare occurrence that one would probably never ever encounter one, but that is probably only true with fully and classically symptomatic cases. We have started looking at abdominal subcutaneous fat as part of our scanning routine, and guess what? This may not be such a rare occurrence at all. Here are some 15-MHz abdominal wall images of a 63-year-old hypothyroid woman who previously had a hysterectomy for a precancerous endometrial polyp:
 |
 |
Her history was interesting, with allergies that began in middle age and episodes of flushing during the past five years that she attributed to "hot flashes."
Who or what is an Aunt Minnie?
I had a chance to meet and spend some time with Ben Felson when I was a resident. This is not a non sequitur. He was one of the great American radiologists of the pre-CT era and perhaps the best radiology educator of his generation. He is the one who coined the term "Aunt Minnie," as long-time readers of AuntMinnie.com may know.
As I recall, he often said that when your Aunt Minnie enters the room, you know right away who she is, even if you don't know how you know. He meant this as a metaphor for learning to recognize some specific patterns of pathology (mainly in chest films) instantly and preconsciously.
Soft, well-demarcated reflective nodules in subcutaneous fat are an Aunt Minnie of a sign. They are not palpable, and I suspect they can only be found by high-frequency ultrasound, which is perfect for outpatient screening applications. There may be a completely unexpected, relatively high prevalence of this finding, and it seems that multiple nodules may predispose several allergic disorders, including conditions such as irritable bowel syndrome (IBS), fibromyalgia, and possibly even exercise-induced asthma or postexertional hypotension and reactive tachycardia.
Mast cells reside in the lung and gut under normal circumstances. Subcutaneous echogenic collections of mast cells increase mediator production and, presumably, the occurrence of symptomatic mediator release, triggered by unrecognized environmental or drug responses, as in Osler's neurasthenic ladies, who became hypotensive and swooned without obvious causes.
Some image considerations
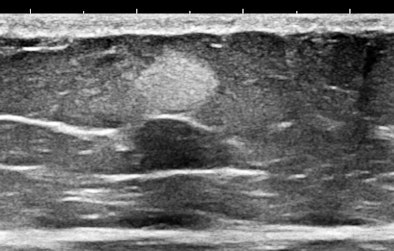
Some of you might think these nodules look like occasional findings in breast ultrasounds that are commonly thought to be lipomas. Lipomas are encapsulated fat, and they are distinguished from fat mainly by their capsular boundary. Here is another type of echogenic nodule, a solid mass of mixed histology with fat, muscle, and vascular components. This type of mass is typically palpable; their firmness is demonstrated by shear-wave elastography:
 |
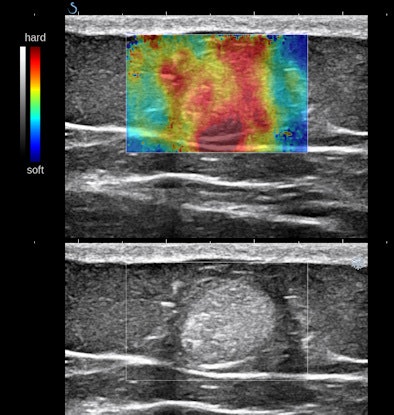 |
The first example is of an infiltrating, multifocal process, such as with leukemia; the second involves stable islands of cells without a supporting macrostructure; and the third is a solid, benign mass. The image features are distinct.
Possible new signs
When you encounter something that seems to be new, the first step is to check the literature. Search engines are a really big help. When that doesn't turn up anything exactly the same, the traditional strategy has been to keep it secret, try to gather a few more cases, and then present it at a meeting or submit it to a journal. There, its fate may be decided by a limited number of reviewers, some of whom may be excessively zealous as fault finders if they suspect that the submitter has ever previously reviewed their works.
Peer review is essential, but it seems foolish in these times of instant mass communication to retain a limited and arbitrary definition of the process for all types of research. That is why I have decided to treat all of the readers of AuntMinnie.com as imaging peers for what appears to be a previously unreported sign: clinically occult, echogenic tumorlike collections of mast cells in subcutaneous fat, detected by superficial scanning with a high-frequency, low-noise ultrasound imaging system.
Announcing a finding is the easy part of a process, and I hope that AuntMinnie.com will become a primary site for sharing new radiologic concepts at their inception. The current system of a scientific paper and subsequent publications for verification, reconfirmation, and utility has been the academic standard for a very long time.
This procedure was perfectly suited to the 19th century when the medical community was small, the knowledge base was limited, and research was the province of a few academic centers, typically with great libraries where their own scholars could leisurely survey the past. It is absolutely necessary to preserve this conservative approach when the topics are procedures or treatments with associated hazards, and especially when the researcher has some kind of vested interest in the proceedings. Perhaps, though, we all need to be more flexible at this point in the burgeoning of the information era and learn to utilize our available resources more effectively.
A democratic research paradigm
Think about this: There are a zillion ultrasound exams done every day, and those doing the exams are always making observations. This has vast research and educational consequences if you have the ability to share those insights and your clinical creativity with your colleagues.
For example, a portion of essentially each of the 10 million fetal exams done each year in the U.S. includes measurements and evaluation of gestational age and growth. Is it optimal or even valid to use standards worked out in the 1970s with a limited number of patients with low-performance equipment from that era? If only a few percent of our ultrasound community pooled its quantitative data with equipment and expertise available now, we would have great standards to use for our daily exams, and the quality of our services and recognition of problems would be improved.
The concept is nonjudgmental scientific collaboration, which is potentially difficult to achieve given a very long history of distrust between physicians and paramedical personnel, of academic centers tending to underestimate the capabilities of community practice, and of the more recent phenomenon of commercial competition between alternate healthcare systems within a limited geographic radius.
Everyone can be a researcher
Here is how you can contribute directly to ultrasound research: I want you to take 30 or 40 seconds for some value-added, extra scanning of anterior abdominal subcutaneous fat with a high-frequency probe when you are doing a clinical ultrasound exam on an adult (particularly women older than 40). Keep track of the patient's age and gender and whether there were zero, few, or many reflective nodules.
I have started a website, datasonics.net, where there will be downloadable permission and data-entry forms, a tutorial, and a mechanism for uploading those data. Anyone or any facility involved in ultrasound examinations can register for free, and all of the data are available and visible to all participants for their own uses. This portal has been self-funded by my practice.
There is also an associated blog, datasonics.net/wordpress, which I hope will be an open forum. I want to invite all of you, and especially my former academic confreres who think of themselves as "researchers," to use this blog as a place to suggest observational research topics for the datasonics network. You will have priority as well as an array of informed comments and very likely a finished large-scale data acquisition in a fraction of the time it used to take. Isn't the information age virtually wonderful?
Why research?
When I was teaching, I always encouraged technologists, residents, and fellows to take on some kind of observational research as part of their hands-on education. When you are looking hard for something, the rest of the exam always turns out to be more thorough. It is a matter of focus and of making a personal investment in the exam.
Research is nothing more than making observations dispassionately and keeping track of and collating those observations and selected other factors. There are probably those who doubt that the general ultrasound community is capable of contributing to our field in this way. My own opinion is that we cannot afford hierarchical snobbery any longer and that our patients deserve nothing less than what we can accomplish equally and together.
Dr. Jason Birnholz is a graduate of Johns Hopkins School of Medicine and did his diagnostic radiology residency at Massachusetts General Hospital. He was awarded an Advanced Academic Fellowship from the James Picker Foundation and has been a professor of radiology.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnie.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.



















