AuntMinnie.com presents the 13th in a series of columns on the practice of ultrasound from Dr. Jason Birnholz, one of the pioneers of this modality.
Fellow Ultrasounder,
With obesity becoming epidemic, liver ultrasound has gone from a core competence to an essential component of nearly every abdominal ultrasound exam on patients ranging from preteens to senior citizens.
I am going to start with fatty infiltration (steatosis) as the most common cause of hepatic inflammation that initiates fibrosis, which may progress to clinical cirrhosis. Recognizing liver fat and fibrosis are quintessential tasks for grayscale diagnostic.
 Dr. Jason Birnholz.
Dr. Jason Birnholz.
Such exams are highly dependent on equipment settings, which is why technical progress in this area has been slow to nonexistent since the 1980s, and why, in desperation, there has been a lot of interest in the ultrasound community recently in various forms of elastography.
My own impression is that if you go with the factory presets for liver imaging of any of the recent scanners, you will only be able to handle extreme forms of these conditions and will completely miss the early diagnostic potential inherent to ultrasound.
I am often amused by scientific papers about various forms of MRI for fatty liver. There is usually some sentence to the effect that ultrasound "may have some use, but it is not quantitative," and then a convoluted analysis ends with a few qualitative categories, just like the traditional form of visual grading typical in radiology and pathology.
We all seem to want simple numerical indices for complex issues, and often this is just not possible or practical. MRI is, of course, a great tool, but it does not have the rapid, low-cost ambulatory screening capabilities that ultrasound practitioners employ in other situations every day.
I am going to show you a platform-independent way to improve your ultrasound images and get a lot more information out of them for free with any old computer that is sitting around idle in your facility (or at home).
Fat
A liver is fatty when there is an accumulation of triglycerides within the cytoplasm of hepatocytes, initially as tiny vesicles, some of which will coalesce into larger globules that may displace the nucleus or otherwise distort the cell. All of these vesicles are, obviously, much smaller than the shortest wavelength for the ultrasound transducers used in clinical practice.
The ultrasound findings are due to changes in the nonspecular components of the signal that influence scatter. The typical appearance is a normal size and shaped liver with a normal-appearing vascular architecture that is bright or "greasy" and for which there is no increase in attenuation.
The parenchyma has a lot of fine speckles, and there is increased noise. Typically there is no problem penetrating down to the kidney; liver is also much brighter than renal parenchyma. If you do not have the gain set too high, you will also notice a ring-down type of enhancement distal to hepatic veins.
When there is a negative gradient in properties such as specific gravity between blood in the vessel and fatty infiltrated liver cells surrounding it, the rounded cross-section of a vessel acts like a converging lens, focusing the beam and promoting an increase in backscatter. That may be kind of subtle, but if you see it and the liver otherwise looks normal, you might want to get that patient back sometime and clue in the referring physician that some lab testing (such as serum triglycerides) might be a good idea.
Why is identifying fatty liver a good idea?
There is an obvious association between obesity and fatty liver. When you get a 300-lb plus patient in, you expect to see a fatty liver, but that isn't always the case. Sometimes you will be shocked by seeing what appears to be a fatty liver in someone whose body mass index (BMI) isn't that elevated and in whom there is no history of excessive and prolonged alcohol consumption or other conditions or drug exposures that may also predispose to steatosis.
The common thought is that fatty liver is part of the metabolic syndrome, which emerges clinically after a decade or more of continued subclinical deterioration. Operationally, I think of fatty liver as causing or promoting metabolic syndrome, because it is usually the first thing that you find ultrasonically.
Most of my patients have been women referred for gynecologic issues, and for whatever reason few of them have had routine lab surveillance including cholesterol, triglycerides, or hemoglobin A1C. Incidentally, fatty liver is much more common in men than women.
Early stages of fatty liver are reversible. When I have chubby patients with an ultrasound finding of a fatty liver, I tell them that people who deposit or accumulate fat in the liver are in a high-risk category of subsequently having hypertension and diabetes and the complications associated with those conditions. They usually embrace weight loss and exercise with a lot more seriousness than they had before.
I suspect that in the future, part of the management of fatty liver, with or without other features of the metabolic syndrome, will include drug therapy with an agent such as a statin to limit the inflammatory component that accelerates the clinical deterioration of these patients. There has also been recent interest in the use of curcumin, an active ingredient of the spice turmeric, as a preventive, but there are problems of bioavailability and dosage that need to be resolved.
A precise definition of fatty liver (as fat at or above 5.5% of liver weight) is mandatory for scientific work, but for clinical decision-making, if there is enough intrahepatic fat to be identified by ultrasound, then there is enough to warrant some kind of preventive health intervention. The incidence of fatty liver is now about 15% of the general population in China and 30% in the U.S.
Nonalcoholic fatty liver disease has been predicted to be the No. 1 disease worldwide in less than a decade. A relatively small percentage of fatty liver patients will go on to fibrosis and cirrhosis, but the burden to any healthcare system from metabolic syndrome and its complications will be very great. A routine ultrasound that includes the liver may be the tip-off that the condition is present at a stage when it is treatable.
Diffuse disease, geographic patterns, ethnicity and genetics
My office referral population is a mix of Caucasian and Hispanic (mainly Mexican) patients with smaller African-American and Asian contingents, mostly but not exclusively women, and mainly adults and not children. In terms of fatty liver, its prevalence is disproportionately higher in Hispanic patients (female and male) than in other ethnic groups. This has also been the observation of several serious studies with large patient populations and precise characterization of liver fat.
The naïve thought is to attribute this to diet, but that would be wrong. Plainly, when there is a gross ethnic variation in disease incidence, there must be a genetic factor (or, as usual, factors). A lot has been learned about the genetics of fatty liver in recent years. It's complicated. One reconfirmed finding is that a single nucleotide polymorphism (SNP) for a gene controlling the oxidation of fatty acids has a singularly high incidence in Hispanic populations.
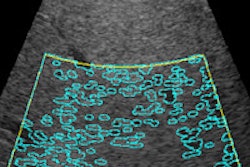
Have a glance at the image below. There is one more related, practical concern for this imaging task. We tend to think of fatty liver as one of the "diffuse" liver diseases, affecting all of the liver uniformly. The first few times you see a rounded, less-reflective "nodule" within a fatty liver, you will assume that this has to be a metastatic lesion, even though the fine detail does not look the way you expect a met to appear.
I can remember doing some ultrasound-guided liver biopsies of such nodules back in the early 1980s. The results always came back "normal liver." Of course we worried that maybe the biopsy missed the lesion, until we learned that these were actually islands of normal liver that had not yet or were somehow resistant to fatty accumulation. The following image has a peripheral zone that has been spared.
 Mild fatty liver in a 42-year-old woman with a more intense patch posteriorly in the right lobe adjacent to spared peripheral patches. All images courtesy of Dr. Jason Birnholz.
Mild fatty liver in a 42-year-old woman with a more intense patch posteriorly in the right lobe adjacent to spared peripheral patches. All images courtesy of Dr. Jason Birnholz.Since the 1990s and mainly via CT scans, it has been known that fatty livers can have a geographic pattern with various zones of fatty and normal tissue. I once saw a right lobe that looked like a yin-yang sign with a bright top and a curved border over a normal lower section. The reason I mention this is that when the issue is an SNP, you will have a diffuse pattern when all of the cells are afflicted and something very different when there is a genetic mosaic.
This has been well-recognized in dermatology, when skin manifestations of systemic diseases occur in patches or along dermatomes. The rash is expressed in those cells having the bad SNP. What this comes down to is a more basic question of how diffuse or geographic an infiltration really is.
This becomes important when we try to sample a small part of the liver with a biopsy or some region-of-interest application such as elastography. How much and how often do we need to sample? You can probably answer that for advanced tumor disease, but it can be tricky for potentially geographic situations such as fatty or fibrotic liver.
Adipocyst activity
I do not intend to say much about the second stage of liver deterioration, which is inflammation. Inflammation per se does not seem to influence ultrasound images appreciably. I suspect that by the time we are reasonably certain of fatty infiltration, there is already some small component of inflammation present and that any changes in the microvasculature are well below Doppler detection thresholds.
Parenthetically, really sensitive Doppler would be a fantastic tool, because fat cells in obesity secrete vasoactive factors that limit blood flow, making the region hypoxic and promoting the release of inflammatory factors, leading to adipocyte hypertrophy. This is contrary to what we expect with inflammation elsewhere in the body.
To me, the major lesson of molecular biology and genomic medicine is how unbelievably complex physiologic and pathophysiologic processes are. Fat cells are as complex as any other. As an imager, if I happen to know that in obesity there are increased circulatory levels of leptin from adipocytes and that leptin promotes cardiac hypertrophy, then I have a reason to include left-ventricular wall thickness in my survey when a patient with a high BMI comes in.
I'm not personally wild about the way the term "holistic" is thrown about, but as imagers concerned with early diagnosis and prevention, I do not think we can afford the luxury of single-organ or single-region viewing.
Obesity is proinflammatory. A lot of molecular and genetic mechanisms have already been identified explaining how inflammatory responses are triggered. For our purposes, we should consider obesity identical to chronic inflammation from some low-level persistent infection. I do not know if fat accumulated in liver cells upregulates or activates proinflammatory genes or whether the changes result from cells bursting, causing a cellularly mediated inflammatory response.
The end result is that a lot of liver fat will eventually lead to inflammation. Within the liver itself, collagen-secreting stellate cells are activated by inflammation. Chronic focal cholecystitis is a pathophysiologic effect on an immediately adjacent organ, which is a big link in the association between obesity for many years and eventual cholelithiasis.
Collagen, collagen, and collagen
There has been a lot of commercial ultrasound attention to the diagnosis of liver fibrosis in the past few years, perhaps because of our current appreciation of the high prevalence of hepatitis C exposure. There are so many plainly healthy obese people around, and the ill consequences of obesity can be far enough removed in time that the popular appreciation of the problems of this condition are somehow considered less pressing than a viral exposure.
No matter what your emotional biases may be about overindulgence in carbohydrates or alcohol or fears of viral hepatitis exposure, the clinically important concern is fibrosis because that can affect the length of life, not just its quality. Our tasks are to identify a risk state (like steatosis) and to grade the presence and extent of fibrosis.
I have always regarded this paper as one of the foundational works for all of ultrasound: Fields S, Dunn F. Correlation of echographic visualizability of tissue with biological composition and physiological state. J Acoust Soc Am. 1973;54(3):809-12. What we are mapping with ultrasound is mainly the bulk modulus of elasticity for the volume elements of our sampling, which is mainly the amount, type, and macrostructure of the collagen endoskeleton of "soft tissues."
Lots of tiny patches of collagen make liver parenchyma appear coarse or heterogeneous and attenuation is increased markedly. What I like to do is to make magnification views of small regions of hepatic parenchyma, usually 5 to 7 MHz per custom and at 15 to 18 MHz when that is practical. Fibrosis is indicated by bright spots in the field-of-view.
If you think about it, elastography is a way to increase tissue contrast at the expense of detail resolution, and there is a composite number (i.e., stiffness) that characterizes an average of this feature. This is fine for large, uniformly abnormal regions. My hesitation about this is that we really want to identify fibrosis when it is microscopic, as in a biopsy.
I suspect that subtle variations in the extent of fibrosis, along with vascular pulsations and breathing, possibly also variations in transducer skin contact, lead to variations in elastographic features when the sampling is repeated multiple times at the same place. Whether we are using radiation pressure or shear-wave elastography, 2D imaging and elastography are both dependent on ultrasound wave propagation. Is there some way of making this common information more visible in conventional images?
Enhancing the diagnostic return of a 2D image
This is the finesse part, but I think this solution is sort of elegant. It uses whatever ultrasound system you have, and it is cheap.
Evaluating fatty and/or fibrotic livers involvesassessing tissue texture, like distinguishing the woven pattern of cloth from the surface pattern of polished marble. There are ways to characterize textures numerically, but they are not simple. On the other hand, the eye and brain handle these second- and third-order 2D statistical distribution tasks instantly and well.
For most of the history of ultrasound, it has not been possible to access the raw reflectivity data from which the image is formed. This dataset has a much broader dynamic range than monitors can display, so the signal is conditioned before it is sent to the display device (previously a TV monitor).
One of the cool things about more recent digital devices is that there is an option for exporting the images, which are data at or prior to the display device in the equipment. On some devices this is as a bitmap (that's best) and for others it is as a compressed JPEG (not preferable, but still pretty good).
What that means is that you can export your images to a jump drive and then bring it to any computer, and what you will be working with is pretty close to raw ultrasonic data and for which there are features that may be perceptible in the visualized display.
The next part is to download one of the best image processing programs you can find: ImageJ (the J is for the Java programming), which is provided for free from the U.S. National Institutes of Health (NIH). I love this program. It is up to version 1.48, there are a lot of routines, and it executes almost instantaneously.
I export liver images into my computer and open them one at a time in ImageJ. I select a region of interest. Often I will alter the brightness and contrast or bit depth before I look at the texture pattern.
This is a simple kind of contrast-enhancing and noise-reducing form of grayscale remapping. The real beauty of this preconditioning of images is in additional semiquantitative routines.
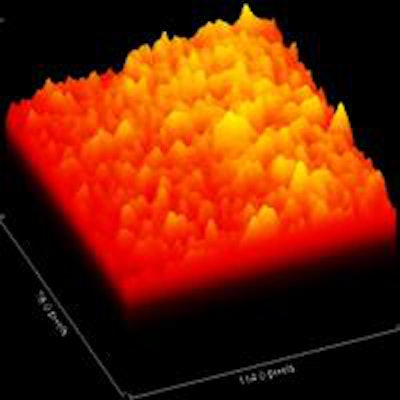
One form of display that I find most helpful in presenting cases to my referring physicians is a 3D picture with signal strength as height. Fatty livers are smooth prairies, while fibrotic ones are mountainous. I also read out the grayscale distribution as a histogram, and I use the 2D Fourier transform option to illustrate visually or to calculate the distributions of spacings between groups of reflectors. I regret that there is not enough space in this column to go into that more fully.
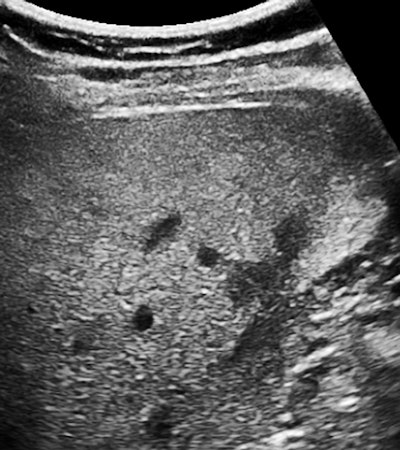
Below are images of another patient.
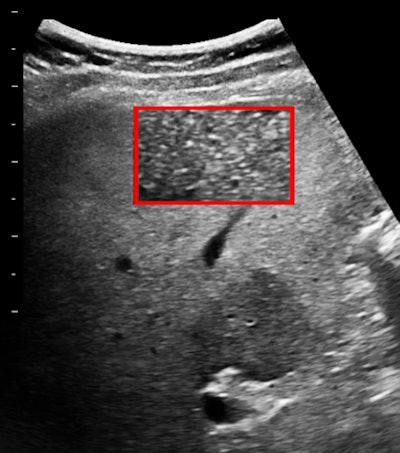 Broadband 6-MHz liver image with a 78 x 114-pixel region of interest.
Broadband 6-MHz liver image with a 78 x 114-pixel region of interest.
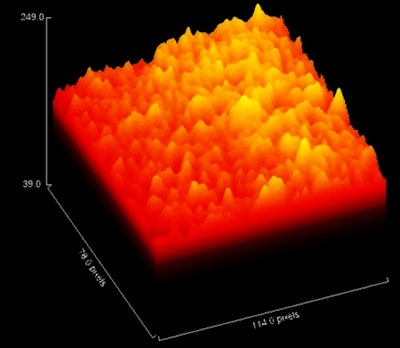 Z-axis display of peak amplitude in the region of interest.
Z-axis display of peak amplitude in the region of interest.
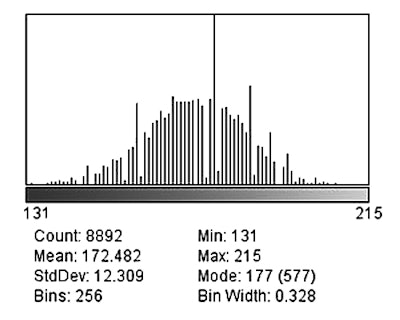 The histogram distribution of grayscale levels in the region of interest.
The histogram distribution of grayscale levels in the region of interest.Conclusion
What have you decided about this case? My report was of fatty liver (with a spared normal region) with the beginning of fibrosis. This was confirmed histologically.
I started a little feasibility project that included 50 patients for whom I was able to get some additional clinical and lab information. There was excellent separation of normal livers, fatty livers, and those with fibrosis on visual criteria alone. The standard deviation in the grayscale histogram was the best single numerical discriminator and grader. Ultrasound elastography was not contributory. To be fair, I was seeing healthy ambulatory outpatients, which is pretty far removed from inpatients with established and advanced liver disease.
At some point, I suppose the manufacturers will start to look at ways of extracting quantitative information from preimage data in conventional scanners. In the meantime, this is a simple way to spiff up your appreciation of grayscale features in images.
What I know is that any techniques or technical tricks that focus you on making the best images and on getting the most info out of them can only make you a better ultrasounder. This is true for any application. Try ImageJ on a region of interest of an anterior placenta with a 15- or 18-MHz probe, for example, and you will make this a part of every third-trimester obstetric exam you do subsequently.
Dr. Jason Birnholz was one of the few advanced academic fellows of the James Picker Foundation, and he has been a professor of radiology and obstetrics. He is a fellow of the American College of Radiology and the Royal College of Radiology, and he was an associate fellow of the American College of Obstetricians and Gynecologists.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnie.com.