Ghost scans -- that is, when point-of-care ultrasound (POCUS) exams are performed but no images are saved -- are problematic and may have haunting consequences, suggest findings published October 24 in the American Journal of Emergency Medicine.
Researchers led by Zachary Boivin, MD, from Yale University in New Haven, CT, found that ghost scanning rates varied across institutions but were still high, ranging from more than one out of five exams to more than nine out of every 10 exams.
“These results show that ghost scanning continues to be a concern in the emergency department and further studies are needed to test interventions to decrease its rates,” Boivin and colleagues wrote.
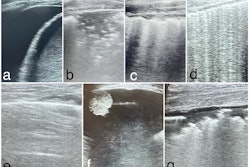
While ghost scanning is common in POCUS, it is understudied, especially regarding direct comparisons between institutions, the investigators noted. In their study, they compared the prevalence of ghost scanning across multiple institutions for patients with trauma activations who received an extended focused assessment with sonography in trauma (eFAST) exam.
The research included four Level I trauma centers with emergency medicine residencies and emergency ultrasound fellowships. The team included data collected between 2021 and 2023. It manually reviewed documents from the electronic medical record (EMR) for eFAST exams and then searched for corresponding saved images.
The study included information from 6,078 patients from the four sites. Of the patients, 2,182 (35%) underwent an eFAST exam for trauma, with rates across the sites ranging from a low of 24.5% to a high of 49%.
The overall scanning rate was 49.8% for the entire cohort, with 1,086 images saved. The team reported a significant difference between all sites when compared as independent pairs (p < 0.001). Ghost scanning rates varied among the study sites.
Ghost scanning rates by study site | |
Study site | Ghost scanning rate |
Site 1 | 33% |
Site 2 | 65.5% |
Site 3 | 21.4% |
Site 4 | 93.2% |
Within each site, the team also compared ghost scanning rates for positive and negative eFAST exams. This analysis excluded any indeterminate exams.
The team observed a statistically significant decrease in ghost scanning rates for positive eFAST exams at site 2 (50.5% positive vs. 70.5% negative exams; p = 0.001). Site 3 had a statistically significant increase in ghost scanning rates for penetrating trauma (50% for penetrating trauma vs. 20.5% for blunt trauma; p = 0.02).
The variation in ghost scanning described in the study “is likely to be related to both workflow differences and workplace practice patterns,” the authors noted.
They outlined other factors that could be considered for this trend.
“Physicians who received limited POCUS training may be less likely to see the value in saving images,” the authors wrote. “Additionally, it is likely ghost scanning rates increase when physicians are faced with a critically ill patient, as other tasks can take priority.”
The team also called for future studies to focus on decreasing ghost scanning through prospective projects on quality assessment and improvement.
Read the full study here.