More stringent diagnostic criteria from the Society of Radiologists in Ultrasound (SRU) for determining early in the first trimester if a pregnancy has no chance of producing a live baby will not lead to a huge increase in follow-up ultrasound exams, researchers from the University of California, San Francisco (UCSF) have found.
In a large, retrospective study published in the September issue of the Journal of Ultrasound in Medicine, a team led by Dr. Maowen Hu found that the new, more conservative criteria for diagnosing nonviable pregnancy on ultrasound would lead to follow-up studies in fewer than one in eight patients.
"While these more stringent guidelines will result in more sonograms in follow-up, the number of additional sonograms does not seem inordinate for the increased safety," senior author Dr. Roy Filly told AuntMinnie.com.
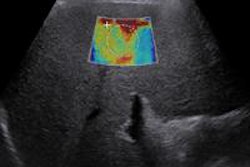
Published in the New England Journal of Medicine in October 2013, the new SRU recommendations set several more stringent conditions for determining that a pregnancy is not viable, including the following:
- An increase in crown-rump length to 7 mm (up from 5 mm previously) for embryos without a heartbeat
- Expansion of mean sac diameter to 26 mm (up from 16 mm previously) for "empty" sacs
The goal of the new criteria was to diagnose failed pregnancy only in cases in which, based on ultrasound findings, the chance of a normal intrauterine gestation was virtually zero. As such, the ultrasound criteria used should have a specificity and positive predictive value as close to 100% as possible, according to the authors.
Because the more stringent criteria would also lead to more follow-up ultrasound studies, "we wanted to make a reasonable estimate of how many sonograms the new proposed 'rules' would engender," said Filly, a professor emeritus at UCSF's department of radiology.
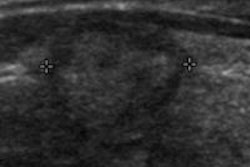
To accomplish this goal, the team retrospectively reviewed all first-trimester ultrasound studies from 1999 through 2008 in women with first-trimester bleeding. A total of 1,013 women were included in the study, all of whom had a visible gestational sac in the uterus. The researchers did not include any pregnancies of an unknown location or ectopic pregnancies (J Ultrasound Med, September 2014, Vol. 33:9, pp. 1585-1588).
Of the 1,013 women, 752 (74%) had identifiable embryos, while the remaining 261 (26%) did not. No detectable embryonic cardiac activity was found in 286 (38%) of those with an identifiable embryo.
Crown-rump lengths for identifiable embryos with no detectable embryonic cardiac activity were as follows:
- Less than 5 mm: 100 women
- 5 to 7 mm: 36 women
- ≥ 7 mm: 150 women
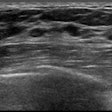
Mean sac diameters in women with identifiable embryos with no detectable embryonic cardiac activity were as follows:
- Less than 16 mm: 120 women
- 16 to 25 mm: 90 women
- ≥ 25 mm: 51 women
As a result, 126 (12%) of the 1,013 women examined for threatened abortion would have been included in the new ranges for recommending a follow-up exam, the researchers concluded.
"Even among those diagnosticians who adopt the more stringent criteria ... an additional examination would be recommended in fewer than one per eight patients," the authors wrote. "Therefore, we conclude that these changes affect a relatively small number of patients and do minimize critical errors and potential harm to a normal intrauterine gestation, a much more important change than the resulting additional medical tests for some patients."
Because the study was designed only to assess the number of follow-up ultrasound studies that would have been performed under the new criteria, patient outcomes were not assessed.
While the UCSF team will not reinvestigate this particular topic, it is planning to evaluate certain ultrasound findings that are suspicious but not currently considered diagnostic of pregnancy failure, Filly said.
"We believe some of these can be elevated to levels of high diagnostic confidence," he said.