Contrast-enhanced ultrasound (CEUS) appears to be an effective alternative to MRI for identifying early cervical cancer -- especially in women who have tumors small enough to make them candidates for surgery, according to a study published in the August issue of Ultrasound in Medicine and Biology.
The study findings offer a way to preserve the fertility of women who are diagnosed with the disease and are still of childbearing age, wrote Dr. Kolbrún Pálsdóttir of the Karolinska Institute and colleague Dr. Elisabeth Epstein of Södersjukhuset, both in Stockholm. MRI has long been used to identify cervical cancer and stage treatment, but it can miss cancers smaller than 2 cm that may be eligible for surgery.
"Ultrasound might be superior to MRI in detecting small tumors (< 1 cm), such as are suitable for fertility-sparing surgery," the researchers wrote.
Better pictures
Imaging is the current gold standard for staging cervical cancer, with MRI as the most commonly used modality. But studies have shown ultrasound to be at least as accurate as MRI in identifying cervical tumors, and perhaps better for finding smaller cancers, Pálsdóttir and Epstein wrote.
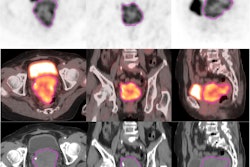
In particular, contrast-enhanced ultrasound offers an additional benefit over color or power Doppler ultrasound in that it can visualize smaller vessels and allow physicians to estimate circulatory changes that may point to cancer activity. But it has remained unclear whether adding CEUS to conventional ultrasound better identifies cervical cancer, so the investigators conducted a study to explore the technology for this application (Ultrasound Med Biol, August 2018, Vol. 44:8, pp. 1664-1671).
"Malignant tumors in the uterine cervix are well-vascularized in contrast to normal cervical stroma," they wrote. "[But] it has not yet been established whether any diagnostic advantage may be gained by adding CEUS to conventional [ultrasound imaging] in patients with cervical cancer."
Pálsdóttir and Epstein tracked both qualitative and semiquantitative parameters to assess the diagnostic accuracy of CEUS compared with conventional ultrasound for cancer tumor detection. The qualitative parameter was contrast distribution (i.e., "filling pattern"), while the semiquantitative parameter was the time intensity curve, or TIC, a measure that shows signal intensity values over time after contrast has been administered. For contrast distribution, the investigators examined both tumor-focused and general contrast patterns.
The study included 49 women with all stages of cervical cancer referred to Karolinska University Hospital for treatment between July 2012 and July 2015, as well as 21 healthy controls. Study participants underwent conventional grayscale and power Doppler ultrasound, followed by CEUS.
Pálsdóttir and Epstein found that ultrasound contrast distribution and TIC quantitative parameters differed significantly between women with healthy cervical tissue and those with cervical cancer. The study showed focal contrast distribution in 89% of women with histologically detectable tumors, compared with 3% of women with no tumors; this focal contrast distribution successfully predicted residual cervical tumor at histology with a positive predictive value of 94%. Their analysis also showed that median peak intensity of the contrast was significantly higher in cancer patients than the controls, in both the maximum intensity area and the whole cervix or tumor.
Finally, the team found that the interobserver reproducibility for assessing focused versus general contrast distribution patterns was high, with a kappa value of 0.91 (a kappa value of 1 represents complete agreement).
"We found a strong correlation between a focal filling pattern and a residual tumor at histology as well as a substantial difference over time in contrast enhancement between tumors and healthy tissue," Pálsdóttir and Epstein concluded. "These results require further clinical validation in a larger prospective series ... [but we] believe that CEUS may become a valuable diagnostic tool to identify those women with early-stage cervical cancer who are suitable candidates for fertility-sparing surgery."