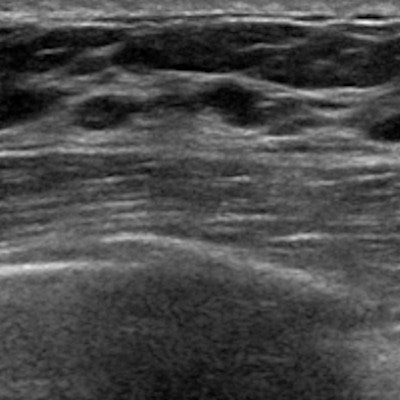
Ultrasound using a shear-wave elastography (SWE) technique can help clinicians determine whether biopsy-confirmed ductal carcinoma in situ (DCIS) should be upgraded to invasive ductal carcinoma, according to a study published online August 1 in the Journal of Ultrasound in Medicine.
Although ultrasound-guided core needle biopsy has long been used as a preoperative tool to assess breast lesions, it can underestimate invasiveness in DCIS -- a problem when it comes to effective treatment, wrote a team led by Dr. Yoon Joo Shin of Seoul National University Bundang Hospital in South Korea.
"Upgrading the histologic diagnosis to invasive cancer can substantially affect the clinical treatment of patients by signaling the need for further axillary node sampling," the group wrote.
Shin and colleagues investigated whether adding shear-wave elastography, which measures lesion elasticity, could improve the performance of ultrasound-guided biopsy in predicting invasive cancer in DCIS lesions.
"In strain or shear-wave elastography, the elasticity value denotes the stiffness of the mass; the stiffer the mass, the higher the probability of it being cancerous," the authors wrote. "In recent times, ultrasound has begun to be used routinely for the evaluation of tumor elasticity to distinguish between BI-RADS category 3 and 4A lesions. Moreover, recent studies have demonstrated that elastographic imaging could help determine the invasiveness of DCIS."
To explore this, the researchers conducted a study that included 80 women with ultrasound-guided biopsy-confirmed DCIS who underwent preoperative mammography, ultrasound, and shear-wave elastography. They reviewed the women's clinical records, pathologic reports, and imaging results and evaluated the final BI-RADS assessment, including the elasticity of the lesion.
Among 80 lesions, 33.8% were found to have an invasive component after surgical excision. The group found that higher BI-RADS assessment categories and nuclear grades correlated with a lesion's invasiveness (p = 0.015 and p = 0.005).
"The probability of a histological upgrade was six times higher in BI-RADS category 5 lesions compared with category 4A lesions ... and three times higher in histologic grade 3 [lesions]," Shin and colleagues wrote.
They also found that maximum SWE stiffness values were higher among women with invasive cancer compared with those who had pure DCIS, at 119.04 versus 85.33.
The study results led the group to conclude that shear-wave elastography can offer helpful additional data for women diagnosed with DCIS via ultrasound-guided biopsy.
"The BI-RADS category based on ultrasound findings, maximum stiffness value on shear-wave elastography, and nuclear grade of DCIS are predictive of invasive components in DCIS," the researchers concluded.