A mammogram-based deep learning model can identify more breast cancers at screening MRI than traditional risk assessment models, according to a study published September 19 in Radiology.
Researchers led by Leslie Lamb, MD, from Massachusetts General Hospital in Boston found a higher cancer detection rate and positive predictive values (PPVs) in patients deemed to be high risk according to the deep learning model than according to the Tyrer-Cuzick model and the National Cancer Institute Breast Cancer Risk Assessment Tool (BCRAT).
“These results … support the use of a deep learning model in clinical practice,” Lamb and colleagues wrote.
Risk assessment models such as Tyrer-Cuzick and BCRAT are used to determine whether women undergoing breast cancer screening should have supplemental MRI performed on them. However, the researchers pointed out that these models have only modest accuracy in predicting breast cancer.
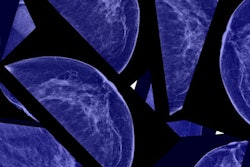
Lamb and co-authors wanted to compare the diagnostic accuracy of a mammogram-based deep learning risk assessment model to that of these traditional risk models in patients who underwent supplemental screening with MRI.
The deep-learning model uses standard 2D mammographic views to predict a patient's five-year risk of developing breast cancer. Images go through an image encoder and an aggregation module to combine information across the views, and from there, the model predicts a patient’s traditional risk factors. The model was trained on 210,819 mammograms, validated on 25,644 mammograms, and tested on 25,855 mammograms.
For the current study, the team included 2,168 women with a median age of 54 years who underwent 4,247 high-risk screening MRI exams. It noted that no mammograms from the current study were used in the model’s development or testing.
The researchers found that the cancer detection rate and PPVs were higher in high-risk patients according to the deep-learning model than according to the Tyrer-Cuzick and BCRAT models. For the PPVs, they analyzed the following: abnormal findings at screening (PPV1), biopsies recommended (PPV2), and biopsies performed (PPV3).
| Comparison between deep-learning, traditional risk models | |||
|---|---|---|---|
| Tyrer-Cuzick | BCRAT | Deep-learning model | |
| Cancer detection rate (per 1,000 exams) | 6 | 6.8 | 20.6 |
| PPV1 | 5% | 5.5% | 14.6% |
| PPV2 | 12.7% | 11.1% | 32.4% |
| PPV3 | 13.5% | 12.5% | 36.4% |
| *All data achieved statistical significance. | |||
The study authors wrote that, along with prospective studies and validation, they anticipate that such a deep learning model could be available for widespread adoption, as well as guidelines supporting its use in clinical practice.
In an accompanying editorial, Min Sun Bae, MD, PhD, from Korea University Ansan Hospital echoed that sentiment, writing that further prospective studies are needed to support personalized breast cancer screening and answer questions about the clinical use of deep learning models.
“The mammographic image itself may contain information associated with an individual’s risk of future breast cancer,” Bae wrote. “This information will be important to improve screening performance. The frequency of screening and supplemental screening with MRI or ultrasound should be more personalized based on individual breast cancer risk.”
The full study can be found here.