June 19 is Juneteenth, a day marking the emancipation of enslaved people in the U.S., and a time to reflect on our progress toward equality and justice.
 Dana Brown, president and CEO of iCAD.
Dana Brown, president and CEO of iCAD.
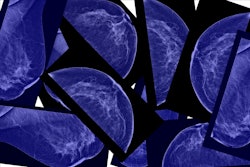
However, it's also a moment to acknowledge the persistent disparities that continue to affect Black communities, particularly in healthcare. One such disparity lies in the realm of breast health, where minoritized groups face disproportionately higher risks of certain aggressive breast cancers and poorer outcomes compared with white women.1-3
Stark disparities
The statistics are sobering: Black women are not only more likely to be diagnosed with breast cancer at younger ages and later stages, but they also have a higher mortality rate. According to recent data from the American Cancer Society, Black women are 40% more likely to die from breast cancer than white women, and this gap widens among younger age groups.4
Moreover, the U.S. Centers for Disease Control and Prevention (CDC) reports that Black women have an 81% higher rate of triple-negative breast cancer, an aggressive subtype that can be more challenging to detect and treat through traditional screening methods.5 This incident rate of triple-negative is particularly concerning in light of the fact that Black women are also given fewer digital breast tomosynthesis (DBT), or 3D, mammograms than other racial and ethnic groups,6-7 even though DBT is better able to detect aggressive cancers, especially when complemented with mammographic AI software.
These disparities are not merely statistical outliers but indicative of systemic issues within our healthcare system. Factors such as limited access to quality care, socioeconomic barriers, and implicit bias in healthcare delivery contribute to these stark inequities.
Opportunity for change
Black women face barriers to receiving the care they need due to lack of representation in the healthcare system, cultural responsiveness, and substandard care. The use of patient navigators, especially those from the Black community, along with enhanced physician education regarding health disparities, could significantly improve breast cancer outcomes for Black women.8-9
Patient navigators serve as critical liaisons, providing culturally sensitive support, facilitating communication between patients and healthcare providers, and helping to navigate the complex healthcare system. They ensure that Black women receive timely screenings, diagnoses, and treatments, which can mitigate delays and improve survival rates. Concurrently, educating physicians about the unique challenges faced by Black women, including the impact of systemic racism and implicit biases, equips healthcare providers with the knowledge and sensitivity necessary to deliver equitable care. And advocating for the inclusion of mammographic AI assessments within breast cancer screenings adds an unbiased layer of informative data as evidenced by studies reviewing AI risk results between white and Black women,10 as AI algorithms focus on image-based learned results, and isn’t biased by the color of the patient’s skin or where she lives.
This dual approach of patient navigation and physician education, including unbiased AI, addresses both the interpersonal and systemic levels of healthcare, fostering an environment where Black women feel heard, respected, and adequately supported throughout their breast cancer journey.
Harnessing AI for health equity
Globally, over 2.3 million women are diagnosed annually with breast cancer, and every 47 seconds someone loses their life to this disease.11 Early detection is key in the fight against breast cancer, where five-year survival rate increases to over 99% for stage 1 disease.12 Yet more than 20% of breast cancers are missed in traditional mammogram screening workflows, leading to advanced, late-stage diagnoses for many breast cancer patients.13
Adding AI detection software into a radiology workflow is proven to improve cancer detection rates, often by more than 23% when compared with traditional non-AI reader workflows.14-16
AI also offers the potential to address disparities and improve outcomes. For AI to achieve this accuracy, AI development processes must prioritize inclusivity and diversity. By ensuring that training datasets used in AI development represent a wide range of racial, ethnic, and geographic backgrounds, AI algorithms can deliver more accurate and equitable results.
With the availability of cloud-based AI technology, geographical barriers are minimized; a mammogram can be uploaded, analyzed by AI and reviewed by a specialized breast radiologist from anywhere in the world. This ensures that high-quality breast cancer screening and expert interpretations are accessible to all women, regardless of their location, thereby promoting equitable healthcare access and outcomes. Inclusivity in AI development and access is critical, ensuring that no community is left behind.
As we commemorate Juneteenth and reflect on a journey toward equality by achieving equity, let us recommit ourselves to addressing healthcare disparities, particularly in breast health. By investing in education, expanding access to care, and harnessing the power of AI with inclusivity at its core, we can create a future where timely diagnosis and effective treatment are not privileges but universal rights. Together, let’s strive towards a world where everyone, regardless of race or background or geography, has the opportunity to live a healthy and fulfilling life.
Dana Brown is the president and CEO of iCAD. The comments and observations expressed are those of the author and do not necessarily reflect the opinions of AuntMinnie.com.
References
- https://www.bcrf.org/blog/black-women-and-breast-cancer-why-disparities-persist-and-how-end-them/
- https://www.komen.org/breast-cancer/risk-factor/race-ethnicity/
- https://www.breastcancer.org/risk/risk-factors/race-ethnicity
- https://www.cancer.org/research/acs-research-news/breast-cancer-death-rates-are-highest-for-black-women-again.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6316530/
- https://www.jacr.org/article/S1546-1440(21)00006-5/fulltext
- https://www.itnonline.com/article/black-women-are-receiving-inferior-breast-screening
- https://ascopubs.org/doi/10.1200/EDBK_319929
- https://www.komen.org/wp-content/uploads/Landscape-Analysis-Exec-Summary.pdf
- https://www.mdpi.com/2072-6694/14/19/4803
- https://www.who.int/news-room/fact-sheets/detail/breast-cancer
- https://www.cancer.org/research/cancer-facts-statistics/breast-cancer-facts-figures.html
- https://pubmed.ncbi.nlm.nih.gov/27918707/
- Schilling, K. Real-World breast cancer screening performance with digital breast tomosynthesis before and after implementation of an artificial intelligence detection system. Research presentation presented at European Congress of Radiology (ECR) 2023; March 1-5, 2023; Vienna, Austria.
- Journal of Breast Imaging, Volume 5, Issue 3, May/June 2023, Pages 258–266, published 31 March 2023
- Madden, C. Real-world breast cancer detection before and after the implementation of an artificial intelligence detection system in a digital breast tomosynthesis (DBT) screening program. Research presentation presented at the Society of Breast Imaging (SBI) 2022; May 16-19, 2022; Savannah, GA