Using digital breast tomosynthesis (DBT) and supplemental MRI yields more benefits but also confers more risks, according to simulation data published August 26 in JAMA Internal Medicine.
Researchers led by Natasha Stout, PhD, from Harvard Medical School in Boston, MA, found that while DBT plus supplemental breast MRI leads to more deaths averted, it also leads to more false-positive recalls and false-positive biopsy recommendations for women of most breast density categories.
“We found that focusing use of supplemental breast MRI for those women with extremely dense breasts, who are about 10% of screen-aged women, has benefits and results in similar risk to benefit trade-offs as mammography alone," Stout told AuntMinnie.com.
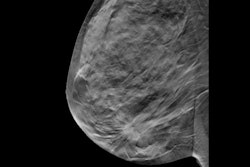
The use of DBT continues to rise in popularity among breast imaging facilities worldwide. But little is known about the long-term benefits and harms of DBT screening with or without supplemental breast MRI, the researchers explained, noting that this information is needed for clinical and policy discussions.
Stout and co-authors sought to project long-term population-based outcomes for breast cancer mammography screening strategies, including DBT and digital mammography, with or without supplemental MRI by breast density. They evaluated starting ages for screening at 40, 45, or 50 through age 74. and used three breast cancer simulation models from the Cancer Intervention and Surveillance Modeling Network (CISNET), informed by U.S. Breast Cancer Surveillance Consortium (BCSC) data.
The results included the following:
- Biennial DBT screening for all simulated women who began screening at age 50 versus 40 averted 7.4 versus 8.5 breast cancer deaths, respectively. It also led to 884 versus 1,392 false-positive recalls and 151 versus 221 false-positive biopsy recommendations, respectively.
- Adding MRI to biennial DBT screening for women aged 50 to 74 years and with extremely dense breasts increased the number of deaths averted to 7.6, the number of false-positive recalls to 919, and the number of false-positive biopsy recommendations to 180.
- Extending supplemental MRI to women with heterogeneously or extremely dense breasts further increased the number of deaths averted to eight, the number of false-positive recalls to 1,088, and the number of false-positive biopsy recommendations to 343.
- The same strategy for women ages 40 to 74 averted 9.5 deaths but led to 1,850 false-positive recalls and 628 false-positive biopsy recommendations.
The team added that biennial digital mammography had similar deaths averted and slightly more false-positive test results compared with biennial DBT screening. Finally, annual screening led to a “modest” increase in estimated deaths averted but increased estimated false-positive results.
The study findings provide critical information considering a recent federal mandate on breast density reporting requirements. Stout said that future research will focus on policy implications of other ways of tailoring supplemental breast MRI use beyond breast density to reach those women who would benefit the most.
"For example, targeting women who are at increased risk of breast cancer for reasons other than breast density or targeting women who are at the highest risk of a cancer missed by mammography might offer opportunities to focus the benefits of MRI," she told AuntMinnie.com. "The NCI-funded Breast Cancer Surveillance Consortium is developing new risk prediction models that may offer opportunities to better tailor screening modalities to those women who would most benefit."
In an accompanying editorial, Ilana Richman, MD, and Tracy Battaglia, MD, both of Yale School of Medicine in New Haven, CT, wrote that understanding questions of access, cost, and equity could affect the population health benefit of supplemental breast MRI.
However, they pointed out that the modeling data in studies such as the one led by Stout and colleagues assume complete adherence to breast screening and equitable access to MRI.
“These assumptions do not reflect realities of the U.S. health care delivery system, and specifically the experience of racially and ethnically diverse populations most at risk for poor outcomes,” Richman and Battaglia wrote. “MRI in particular is an expensive resource that is not universally available or covered by health insurance, and disparities in use have already been described.”
The full study can be found here.