Interobserver agreement is moderate among radiologists when classifying uterine fibroids on MRI, according to research published October 10 in Fertility and Sterility.
A team led by Cibele Luna, MD, from the University of Miami in Florida, found that radiologists using the International Federation of Gynecology and Obstetrics (FIGO) classification system had varying levels of agreement for uterine fibroid types.
“These findings underscore the need for further validation and potential refinement of the FIGO classification system to ensure reproducibility across clinical practice,” Luna and colleagues wrote.
FIGO classification helps categorize uterine fibroids based on their relationship to endometrial and serosal surfaces. Stratification by fibroid type is clinically meaningful since it influences surgical management.
The researchers noted a lack of data on the FIGO classification’s reproducibility when applied to MRI by radiologists with various levels of experience. Luna et al added to the literature with their study of 40 women who underwent pelvic MRI at a single academic institution.
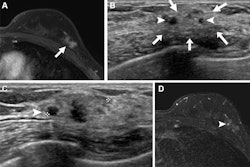
Four radiologists independently reviewed the images and assigned a FIGO classification. The team provided a reference diagram of the FIGO system to the radiologists. The radiologists consisted of two abdominal imaging fellows and two fellowship-trained abdominal radiologists with two to six years of experience. They also provided a confidence score using a five-point Likert scale.
The radiologists achieved moderate overall interobserver agreement (K = 0.461) for FIGO classification. However, agreement varied by subtype. The radiologists achieved substantial agreement for evaluating submucosal fibroids (K = 0.73) and sub-serosal fibroids (K = 0.693). However, they achieved lower agreement for hybrid and intramural fibroids, with K values of 0.387 and 0.33, respectively.
The most common disagreements occurred between FIGO types 2 and 3. This especially went for cases where multiple fibroids distorted the uterine cavity or when fibroids occupied multiple anatomical compartments.
Finally, the team reported no statistically significant difference in confidence scores between radiologists with different levels of experience (p = 0.9).
The authors suggested that while the FIGO system is valuable in categorizing fibroid location, its application to MRI may be limited, especially in complex or ambiguous cases.
They added that future multicenter studies “could refine classification systems, assess ultrasound or intraoperative imaging, and explore subtype-specific assessment with an ‘unclassifiable’ category.'”
Read the full study here.