For women who have undergone breast cancer treatment, FDG-PET proved equal to conventional imaging for patient follow-up, in some cases improving on the results of traditional modalities, such as mammography and MRI, according to an article in the latest issue of the Journal of Nuclear Medicine.
Dr. Duska Vranjesevic and colleagues from the UCLA School of Medicine reported the results of their study on the value of whole-body FDG-PET for determining outcomes in previously treated breast cancer patients. Researchers from the Northern California PET Imaging Center in Sacramento also worked on this retrospective study.
"Breast cancer patients commonly undergo numerous imaging studies after initial treatment even though the therapeutic options for patients with recurrent or residual disease are limited. Nevertheless, detection of local recurrence and metastatic disease can impact therapy," the authors wrote (JNM, March 2002, Vol.34:3, pp. 325-329).
For this study, 61 women were enrolled. The initial histopathologic diagnosis in the majority of these patients was infiltrating ductal carcinoma. For nearly 70% of the women, clinical whole-body FDG-PET was ordered for residual or recurrent disease without any specified reason. Increasing levels of serum tumor markers necessitated the exam in 16.4% cases. The follow-up period after the PET scan averaged 21 months.
Patients received an intravenous injection of 370-555 MBq 18F-FDG; the PET scan was performed on either an ECAT Exact BGO-based PET camera or Exact HR+ BGO-based premium camera (CTI, Knoxville, TN). Images were acquired over 6-9 bed positions. The conventional imaging (CI) procedures were whole-body bone scans, chest CT, abdominopelvic CT, chest x-ray, breast MRI, ultrasound, and mammography.
At the time of final follow-up, 62% of the patients had clinical evidence of stable or progressive disease. According to the results, FDG-PET showed negative findings in 31.1% of the women and evidence of disease in 68.9%. Similarly, conventional imaging yielded negative results in 36% of the cases and positive findings in 64%. PET and the traditional modalities were concordant in 75% cases, with all positive cases (33) deemed true-positive and all negative cases (10), true-negative.
 |
"Blind PET evaluation yielded a sensitivity of 93% versus 79% for conventional imaging (p<0.05). The specificity tended to be higher for PET than for CI (84% versus 68%). The positive predictive value (PPV) of PET was similar to that of CI (93% versus 85%)," the authors said.
However, the negative predictive value (84%) of PET was "significantly higher" than that of conventional imaging (59%) as was the predictive accuracy (80% versus 75%). In addition, when there was disagreement between conventional imaging and PET, the latter correctly predicted the clinical outcome in 80% of these cases while the traditional modalities were correct in 20% of them.
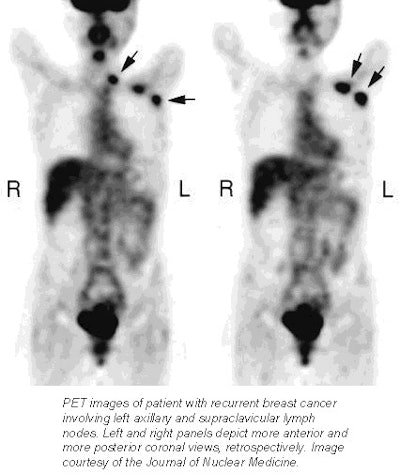
"PET yielded a significantly higher sensitivity than CI attributed to the larger number of false-negative results in CI. In six CI-negative cases, PET revealed recurrence," including axillary and supraclavicular nodes and bone metastases.
"These results support previous studies that showed that lymph node metastasis and bone metastases are detected more often on FDG-PET than on CT or MRI," the authors concluded.
The retrospective nature of this study was one of its limitations, the authors said; as was the three-month time lapse between conventional imaging and the PET exam (disease may have recurred during that interval). The authors addressed this issue by narrowing the time interval between imaging tests to six weeks in 32 patients. They found that PET still had a higher PPV (95%), negative predictive value (90%), and accuracy (94%).
By Shalmali PalAuntMinnie.com staff writer
March 8, 2002
Related Reading
New HOPPS rates bring PET reimbursement hike, March 4, 2002
CMS expands PET coverage to breast cancer patients, February 28, 2002
PET offers important benefits in breast cancer imaging, October 29, 2001
FDG-PET gains favor among referring doctors for cancer staging, treatment, June 7, 2000
Copyright © 2002 AuntMinnie.com