This article is the first in AuntMinnie’s Technology Review series, which examines important medical imaging technologies and their applicability to daily clinical practice.
Although conventional x-ray mammography has recently come under fire, it remains the gold standard for early cancer screening. Mammograms detect up to 85% of all breast cancers, and they are the only exams approved by the Food and Drug Administration for screening women with no signs of the disease.
But what about the remaining 15%-20% of cancers that go undetected? In an effort to catch these cancers, more and more companies are developing computer-aided detection (CAD) technology aimed at assisting radiologists in their film readings. Although radiologists have been skeptical about CAD technology in the past, clinical studies have begun to demonstrate that when trained doctors perform film readings in conjunction with a CAD device, they find more early cancers.
In a study last year, Dr. Timothy Freer of the Women’s Diagnostic and Breast Health Center in Plano, TX, discovered that CAD increases the detection rate of early-stage cancers without generating unnecessary recalls. Freer and his colleague, Dr. Michael Ulissey, screened almost 13,000 women over the course of a year, using both conventional mammography reading techniques as well as CAD, and found almost 20% more cancers than they would have without using the CAD device (Radiology, September 2001, Vol. 220:3, pp.781-786).
CAD’s early days
Researchers began exploring CAD technology in the early 1980s, but were limited by computer horsepower at the time. In 1982, Kunio Doi, Ph.D. and others at the University of Chicago published a study on the use of CAD with mammography x-rays, using a drum film scanner that Fuji Medical Systems had produced. However, initial attempts proved that the ability of computers to convert analog film information to digital data wasn’t sufficient to adequately analyze mammograms, and wasn’t fast enough to be practical at breast imaging centers.
As computer technology caught up with CAD, however, the theory became more of a reality. In 1998, R2 Technology of Los Altos, CA, became the first CAD product to hit the market when it received premarket approval (PMA) from the FDA for ImageChecker, a CAD device used with x-ray mammography.
In the past year, two other firms, CADx Medical Systems of Laval, Quebec, and Intelligent Systems Software (ISSI) of Clearwater, FL, have received approvals from the FDA for their systems. These systems all work with digitized analog mammography film, but most CAD companies are working on versions of their systems that will accept data from full-field digital mammography (FFDM) units.
Although potential users have been doubtful of the technology, in part because of its cost, reimbursement victories early this year have made CAD technology increasingly viable for imaging centers with throughput of at least 20 mammography exams per day.
Clinical applications
Radiologists make thousands of diagnostic decisions every day, and are subject to fatigue, interruptions, and less-than-ideal work environments. Proponents of CAD technology claim that, while CAD is not intended to replace a trained radiologist, it can help doctors do their jobs even better than they already do.
In a healthcare environment that has become increasingly vulnerable to litigation and increased costs, clinical aids such as CAD may prove increasingly invaluable, according to Dr. Peter Shile of the Susan G. Komen Breast Center in Peoria, IL. The Komen Center reads between 100 and 120 mammograms per day.
"As CAD’s benefits become more firmly established, it will be harder and harder to justify (not using it), just like it would be hard for a radiologist to justify not using a magnifying glass when reading films," Shile said.
Currently, FDA-approved CAD technology is primarily being used in conjunction with mammography, although one vendor, Deus Technologies of Rockville, MD, has received clearance for use of CAD with chest x-rays for lung cancer screening. Other applications of interest to CAD developers and radiologists are screening for colon cancer and tuberculosis; other modalities of interest include CT and digital radiography.
CAD and workflow
Breast centers incorporate CAD devices into their work areas differently, depending on their size and the particular device configuration they’ve purchased. Some facilities have a separate room for the CAD device, while others install the unit in their existing reading rooms. A film librarian, technologist, or radiologist feeds a mammogram into the CAD device, which converts it into a digital image via a film scanner built into the system.
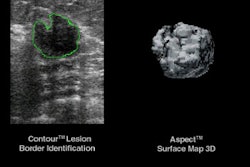
The device then uses computer image-analysis algorithms to detect suspicious characteristics in breast tissue that are associated with cancer -- microcalcifications, or small calcium deposits, and spiculations, or dense regions of radiating lines that indicate a mass. These areas are marked with arrows, asterisks, or some other type of symbol. The marked image is then displayed on a computer screen or hard-copy printout for the radiologist to reexamine.
CAD users told AuntMinnie.com that adding CAD analysis to mammography exams had little impact on the facility’s workflow, adding a mere 7-18 seconds of review time for the radiologist, and between 4-6 minutes extra time to process a mammogram through a CAD device.
The technology is being used at the point of screening and for further evaluation of suspicious mammograms, according to Freer.
"We use CAD to complete the screening exam of every woman we see, whether she’s having a routine screen or whether we’re already concerned about a problem," he said. "But in a sense, every diagnostic patient is also a screening patient, in that there’s at least as much probability that they have a hidden cancer as cancer in the areas we’re already worried about."
Features and benefits
Other than being competitively priced, industry analysts, clinicians, and equipment developers agree that CAD technology must have the following characteristics:
- Be sensitive enough to detect a high rate of cancers.
- Be specific enough to give users information that won’t cause unnecessary workups.
- Be quick and easy to use.
Existing CAD technology tends to be very sensitive, picking up any feature that resembles breast cancer. The technology’s specificity is directly linked to the radiologist’s second reading: When a doctor rechecks suspicious lesions that a CAD device has marked, both the radiologist and the CAD technology work together to produce the 20% increase in early-cancer detection rates, according to the Freer study.
Most CAD devices use pattern-recognition software based on neural networks, with the exception of Mammex TR (Scanis, Foster City, CA), which uses rule-based algorithms.
All devices either on the market or under development also offer both a hard- and soft-copy option for displaying the checked results from a mammogram.
CADx Medical Systems offers Second Look, which analyzes digitized films and prints what the company calls a Mammagraph, with areas of interest indicated.
Deus Technologies markets RapidScreen RS-2000, which analyzes chest x-rays with pattern recognition algorithms, checking for any of 87 features associated with pulmonary nodules, before circling areas of interest in both soft display and the printed image. ISSI’s basic unit, MammoReader, consists of a scanner and a touch-screen reviewer station; clients can add options as needed.
With its ImageChecker device, R2 Technology offers an interactive touch-screen, two kinds of processor units, display units with mini-monitors, and an online viewing option that can be integrated with one or more ImageChecker processing units.
Scanis’ Mammex TR includes an x-ray film digitizer, flat-panel display, a printer, image archiving, and a patient report function.
The features a facility requires in a CAD unit depend on its size and throughput, according to Michele Royston, chief operating officer of Foster & Gross, a small outpatient imaging facility in Laurel Springs, NJ. Royston purchased a basic ImageChecker CAD device from R2 in July of 2001, tailoring the technology to her center’s existing resources and needs.
"We had financial and size constraints, so we set up the basic (ImageChecker) unit right next to our existing lightboxes," Royston said. "It’s not as fancy, but we’re able to move patients through just as well."
Click here for a list of CAD vendors.Competitive technologies
There is currently no competitive technology to CAD, either in the market or on the horizon. Second reading by radiologists could be considered competitive, but second reading is costly and time-intensive, and some breast centers would be happy to retire the practice should CAD prove its value.
Indeed, CAD looks to be the beneficiary of a growing trend in medical imaging: more powerful scanners that produce ever-increasing amounts of data. These systems -- multislice CT is one example -- produce far more images than can be reviewed by any single radiologist. With its ability to scan massive amounts of data automatically, CAD offers a solution to harried radiology practices.
Reimbursement status
In November, the Centers for Medicare and Medicaid Services (CMS) increased reimbursement rates for screening mammography CAD to $17.74 (this amount is in addition to the rate for the screening exam itself). Of this total, $14.48 is for technical fees and $3.26 for professional fees. There are currently no reimbursement codes for any other CAD applications.
Also last fall, the American Medical Association (AMA) issued a separate CPT code for CAD (76085), which, as of January, is to be used as an add-on code with the screening mammography code (76092). The new CAD reimbursement amount represents an 18% overall increase over levels established in April 2001, and a 45% increase for the technical portion.
Some private payors have followed suit. But for those patients not covered by either Medicare or a private carrier that pays for CAD, many imaging centers have collected upfront fees, while at the same time working to educate patients and carriers about the usefulness of the technology in an attempt to increase the pool of coverage.
"Women are demanding CAD, and the clinical community wants to provide it. But we also have to pay for it," Royston said. "At our center, we’ve tried to put the responsibility back onto the consumer to get their insurance carriers involved."
Return on investment
According to vendors and facilities using CAD technology, the break-even point for performing CAD analysis seems to be between 15 and 20 mammograms per day, depending on a center’s Medicare/private insurance carrier mix and the cost of the system purchased.
Foster & Gross spent approximately $350,000 on two CAD units in 2001, basing its purchase on the number of Medicare patients the facility cared for on a monthly basis, according to Royston. CAD reimbursement levels in New Jersey were $15.01 at the time the units were purchased. In addition to charging $39 upfront from patients not covered by Medicare or a participating private carrier, the center has launched an intensive patient/insurer education effort to encourage coverage. After six months of use, Foster & Gross’ return on investment has been $63,000, Royston said.
Freer’s facility bought two systems at list prices ranging from $180,000 to $200,000 each, and now charges women without Medicare $20 upfront for CAD analysis. The center then files the claim with the woman’s carrier, and if it receives reimbursement, refunds the charge to the patient.
Freer’s center reads between 100 to 140 mammograms per day. With the new levels of Medicare reimbursement, Freer is hopeful that the technology will become increasingly viable for most facilities.
"CAD is appropriate for every center, but hasn't been necessarily affordable up to this point," he said. "A center needs to do 15 to 18 mammograms a day to break even, and the majority of facilities in the U.S. don't do that kind of volume. But since January 1, payments under the CPT code for CAD have been very good, even with commercial insurance carriers. We're continuing to monitor the payments, and, if the trend holds, we will discontinue charging our patients, provide CAD to all, and file claims for collection for our CAD exams."
The future
CAD technology will only become more prominent in the future, according to Anthony Montagnolo of ECRI, a Plymouth Meeting, PA, independent nonprofit healthcare research agency. Although cost is still an issue, particularly for smaller imaging centers, CAD will continue to gain clinical acceptance, and patients will continue to demand it.
"Although we don’t know what the technology’s trajectory will be, it will become increasingly difficult to argue with the logic of using it with mammography," Montagnolo said.
CAD technology may prove a boon to radiology overall, not just breast imaging. The technology will mature as developers explore its use with other applications and modalities, and will become more useful in situations where there are a lot of clinical data that need to be interpreted.
"We’re just starting to see the tip of the iceberg," Freer said. "CAD’s applications are far-ranging, and it will become an increasingly important part of radiology in general."
By Kate Madden YeeAuntMinnie.com contributing writer
March 14, 2002
Related Reading
ECR studies explore CAD in breast screening, March 1, 2002
CAD cuts false negatives, increases sensitivity of breast imaging, November 28, 2001
CAD wins over mammographers, October 10, 2001
New CPT code could open door for greater CAD adoption, July 31, 2001
Breast CAD system scores high sensitivity, lower specificity, March 5, 2001
Microcalcifications can’t escape CAD-enhanced mammography, November 29, 2000
Copyright © 2002 AuntMinnie.com