In women with markedly dense breasts, mammography can fail to show more than half of all cancer. Women with mammographically dense breasts may have a sixfold increase in cancer risk, partly because the presence of more tissue means more "room" for cancer to grow. Can advanced imaging techniques, such as computer-aided detection (CAD), cut through this density and pinpoint cancers? Yes, according to a study in the latest issue of the American Journal of Roentgenology.
In a second study appearing in Radiology, Dutch radiologists used matched computer analysis with MR results for characterizing breast lesions. They declared computerized analysis to be complementary to clinical breast MR, possibly increasing the modality's performance for finding mammographically occult lesions.
CAD and breast density
In the AJR paper, researchers from George Washington University in Washington, DC, evaluated the impact of breast density on CAD performance. This study was conducted at 18 institutions across the U.S. The data consisted of 906 mammographically screened cases and 147 normal cases.
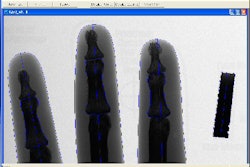
The films were evaluated with the Second Look CAD system (iCAD, Nashua, NH), and digitized using a CCD digitizer with 12 bits of grayscale and resolution of 43 µ. Lead author Dr. Rachel Brem is a stockholder in iCAD, while three of her co-authors are employees of iCAD.
Of the 906 cancer cases, the majority (45%) were classified as scattered fibroglandular tissue, while the minority (8%) were deemed extremely dense. Among the 147 normal cases, 53% were scattered fibroglandular and 9% were extremely dense.
According to the results, CAD detected 89% of the cancer cases (809 of 906). In nondense breasts, CAD found 90% of the cancers (455 of 505). In dense breasts, it spotted 88% (354 of 401). The CAD also detected 93% of the mirocalcifications in nondense breasts and 95% in dense breasts. With regard to masses, the CAD system spotted 89% in nondense breasts and 83% in dense breasts.
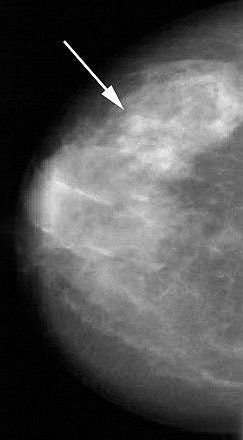 |
| Forty-five-year-old asymptomatic woman. Above, in left craniocaudal mammogram, arrow indicates mass in dense breast. Below, in left mediolateral oblique mammogram, arrow indicates mass in dense breast. Brem RF, Hoffmeister JW, Rapelyea JA, Zisman G, Mohtashemi K, Jindal G, DiSimio MP, Rogers, SK, "Impact of Breast Density on Computer-Aided Detection for Breast Cancer," (AJR 2005; 184: 439-444). |
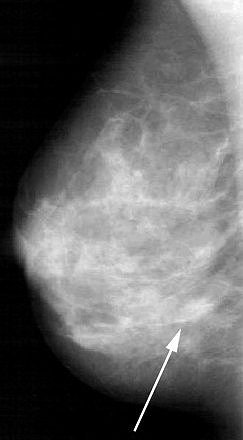 |
This difference in CAD performance for dense and nondense breasts is significant because "CAD detection of masses is lower in dense breasts because of the greater 'background noise' and similar density of masses to the surrounding parenchymal density," the authors explained (AJR, February 2005, Vol. 184:2, pp. 439-444).
In the normal cases, the mean number of false-positive CAD marks per case was 3.35 in dense breasts (0.75 microcalcifications; 2.60 masses). The authors stated that these false-positive rates did not impact the workup rate. "The function of CAD is to point out potential areas of concern to the radiologist," they stressed. "The radiologist makes the final decision (about workup)."
The group concluded that CAD can improve cancer detection regardless of breast density. CAD did prove to be more valuable for microcalcifications, but still performed well in masses. They urged the continued development of CAD algorithms for finding malignant masses.
CAD and breast MR
Given breast MR's high sensitivity and ability to detect incidental enhancing lesions, creating methods to improve the modality's aptitude for distinguishing benign from malignant is important.
"Additional findings at MR imaging are reported in approximately 29% of patients, particularly in young premenopausal women with dense breast parenchyma," explained Dr. Eline Deurloo and colleagues from the Netherlands Cancer Institute and Antoni van Leeuwenhoek Hospital in Amsterdam (Radiology, January 13, 2005).
However, the costly and invasive methods used to diagnose these additional lesions -- either US-guided fine-needle aspiration biopsy or MR-guided core-needle biopsy -- offer a low 3% yield on malignant results, they added.
This group's latest study builds on a previous paper, which reported the effectiveness of a fully computerized system for characterizing lesions on breast MR. In that study, they found that the computer analysis approach significantly improved the modality's performance (Radiology, December 2002, Vol. 225:3, pp. 907-916).
For this investigation, they looked at whether the computerized analysis matched the clinical reading by the radiologist. The study design consisted of four steps:
- Updating the existing system for computerized analysis with an expanded training set and testing
- Evaluating clinical reads of breast MR for lesion characterizations
- Combining results of computerized analysis with clinical reading
- Assessing the performance of that combined model
Contrast-enhanced MRI was performed on a 1.5-tesla unit (Magnetom, Siemens Medical Solutions, Erlangen, Germany) with a dedicated phased-array bilateral breast coil. Only lesions that were smaller than 4 cm3 in volume were included. In total, the data consisted of 236 consecutive lesions (symptomatic or incidental) in 189 patients.
Radiologists interpreted the MR images either on hard copy or on a viewing station. The readers then rated the lesions as benign, indeterminate, highly suggestive of malignancy, etc. The authors pointed out that this study was performed prior to the release of the BI-RADS lexicon for breast MR by the American College of Radiology.
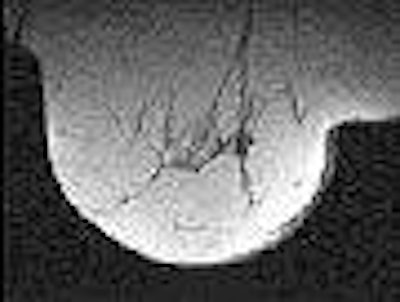
 |
| Transverse MR images of the right breast of a woman who underwent MR imaging for screening because of an increased lifetime risk. Unenhanced (above) and contrast-enhanced (below) images show incidental enhancing lesion of 12 mm, rated indeterminate by the radiologist. Images at US performed for correlation showed no abnormalities. At follow-up MR imaging, the lesion was no longer visible. The combined model calculated a 9.7% probability of malignancy. Fig 4a-b. Deurloo, EE, Muller SH, Peterse JL, Besnard APE, Gilhuijs KGA, "Clinically and Mammographically Occult Breast Lesions on MR Images: Potential Effect of Computerized Assessment on Clinical Reading," Radiology doi: 10.1148/radiol.2343031580. Published online January 13, 2005. |
 |
"A point in the lesion detected by the radiologist is first designated manually on the image," the authors said, explaining how the computerized analysis worked. "The system then automatically shifts the designated point to the center of the contrast-enhanced area, and automatically segments the lesion in three dimensions." Morphologic and temporal features in and around this segmented lesion are automatically rated. The probability of malignancy was based on four features: washout, smoothness of contrast material, mean margin sharpness, and variation in margin sharpness.
According to the results, the computerized analysis complemented clinical reading in characterizing lesions that were rated indeterminate or suspicious by the radiologist. A lesion tagged indeterminate by the reader, but marked as malignant by the computerized analysis, had a high probability of malignancy. The same held true for low probability ratings.
While the performance of clinical reading and computerized analysis was identical (area under ROC curve = 0.86 and 0.85, respectively), the combined model proved significantly better (area under ROC curve = 0.91).
Deurloo's group acknowledged that the study does come with some caveats. Despite the positive results, they did not advise that FNA or biopsy be replaced with computerized analysis in indeterminate or suspicious lesions. In addition, their study design did not account for variability among readers, which is more likely in a real clinical setting.
Instead, they recommended that radiologists consider computerized analysis as a second opinion. "If radiologists always adhere to their initial judgment or always rely on computerized analysis, their overall performance will be comparable but inferior to that possible if they favor only the results of computerized analysis...."
As Brem's group did, these authors also emphasized that "the decision to accept the interpretation of the computerized analysis system has always been at the discretion of the radiologist."
By Shalmali Pal
AuntMinnie.com staff writer
March 15, 2005
Related Reading
iCAD releases Second Look 700, January 27, 2005
CAD systems show double-digit growth in Europe, November 23, 2004
CAD may unmask unsuspected cancers in diagnostic mammo, October 27, 2004
Copyright © 2005 AuntMinnie.com