VIENNA - As women with second breast cancers larger than 2 cm have a poorer prognosis than those with smaller tumors, the practice of surveillance mammography following breast cancer treatment appears to be justified, according to research presented Friday at the European Congress of Radiology (ECR).
In a retrospective review of women with second cancers over a 17-year period, a U.K. research team found that second cancers greater than 2 cm in diameter were associated with a significantly higher risk of death.
"This suggests -- although it's a big leap of faith -- that mammographic surveillance is justified, because as yet we have no evidence that is the case," said presenter Dr. Fiona Gilbert, of the University of Aberdeen's Aberdeen Biomedical Imaging Center in Scotland. She presented the study on behalf of lead author Graeme MacLennan.
Although one in nine women will develop breast cancer over her lifetime, improved treatment has led to more women surviving and living with breast cancer. The effect on follow-up services for healthcare systems is enormous, Gilbert said.
In the U.K. alone, more than 550,000 women -- approximately 12% of the adult female population -- have received breast cancer treatment and are alive, Gilbert said. However, guidelines for surveillance mammography are inconsistent, owing to the lack of robust evidence for this field. No randomized, controlled trials of mammography surveillance have been performed.
The researchers were able to secure funding from the U.K.'s National Institute for Health Research Health Technology Assessment (HTA) program to investigate the clinical effectiveness and cost-effectiveness of mammographic surveillance regimens. The premise is that surveillance mammography reduces the size of second breast cancers that are detected.
To assess the prognostic effect of size of second breast cancer events on survival, the researchers studied two cohorts of women from the West Midlands Cancer Intelligence Unit breast cancer registry. One cohort included women with ipsilateral breast tumor recurrence (IBTR), while the second included women with metachronous contralateral breast cancer (MCBC).
There were 1,174 women in the IBTR cohort, with an aggregate of 3,870 years of follow-up. The median time for diagnosis of the first breast cancer to the second was 41 months. There were 630 overall deaths in this cohort, including 442 known breast cancer deaths.
The MCBC cohort included 975 women, with an aggregate of 4,268 years of follow-up. The median time of diagnosis of the contralateral breast cancer from first to second cancer was 55 months. There were 358 overall deaths in this group, but only 23 known breast cancer deaths.
The researchers used Cox regression models to examine survival in women with second cancers diagnosed between January 1, 1990, and January 31, 2007, adjusting for known risk factors from their first breast cancer. They recorded the length of time from the first tumor until the second tumor (< 60 months or ≥ 60 months) and the second tumor size (≤ 1 cm, > 1 cm to < 2 cm, ≥ 2 cm, or unknown).
In both patient groups, women with breast cancers smaller than 1 cm in size or between 1 cm and 2 cm had much better survival rates than those with tumors larger than 2 cm. An adverse effect on survival was also seen in patients who had less than 60 months to their second breast cancer, Gilbert said.
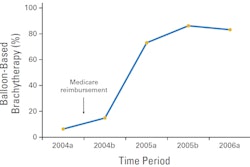
Hazard ratios (95% confidence interval) for all-cause mortality
|
"A larger size of second tumor of more than 2 cm is an indicator of poorer survival, whether it's an ipsilateral breast cancer or a metachronous breast cancer," she said.
Gilbert noted that their results should be interpreted with some degree of caution, as survival from diagnosis is likely subject to both lead and length time biases. She recommended that a randomized, controlled trial be performed, comparing the frequency of mammography.
"We could [also] consider other imaging modalities," she said.