Digital breast tomosynthesis (DBT) is comparable to or better than conventional digital mammography at identifying microcalcifications in up to 95% of cases, according to research presented at this month's American Roentgen Ray Society (ARRS) meeting in Chicago.
The data contradict earlier clinical trials with DBT regarding microcalcifications, said lead researcher Dr. Stamatia Destounis from Elizabeth Wende Breast Care.
"Initial studies with DBT found that the technology didn't see microcalcifications very well and, rather, did better identifying masses," she said. "Perhaps our data showing that it is comparable to digital mammography in finding microcalcifications is due to the fact that the technology has evolved and people are more familiar with how to read the images."
The study included 103 women who had mammograms categorized as BI-RADS 4 or 5 because of microcalcifications. All of the women had a combination exam, which included both conventional full-field digital mammography and DBT in the craniocaudal and mediolateral oblique views.
Radiologists compared image quality, including how visible the lesion was using both modalities, and recorded data that included patient demographics, breast density, size of lesion on both digital mammography and DBT, characterization of the lesion, the biopsy method, biopsy needle gauge, biopsy pathology, and surgical pathology.
Of the 103 women, breast tissue composition consisted of the following:
- 1% (n = 1) fatty
- 30% (n = 31) scattered
- 44% (n = 45) heterogeneously dense
- 25% (n = 26) dense
The average lesion size on DBT was 18 mm, while the average lesion size on digital mammography was 16 mm, according to Destounis. DBT did not find any additional lesions.
The study showed that the quality of tomosynthesis was equivalent or superior to digital mammography in 95% of the cases, Destounis said. She attributed the five cases for which digital mammography performed better than DBT to the learning curve for readers, especially with very small microcalcifications.
"2D was better than DBT in those five cases due to smudgy calcifications," she said. "As you're scrolling through [the DBT image], you have to make your slab pieces smaller or bigger, and if you're cutting too thin, you may not get a true representation of the calcification. In some cases the calcium was so fine, so little, that digital mammography gave a better look at it."
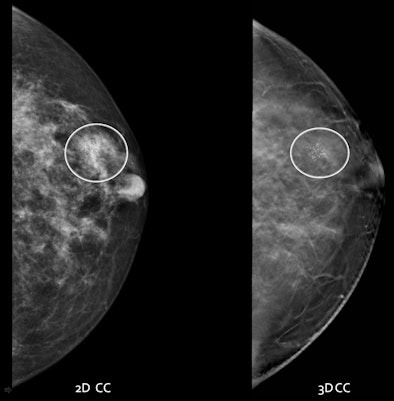 |
| Digital mammography and DBT, craniocaudal view. Images courtesy of Dr. Stamatia Destounis. |
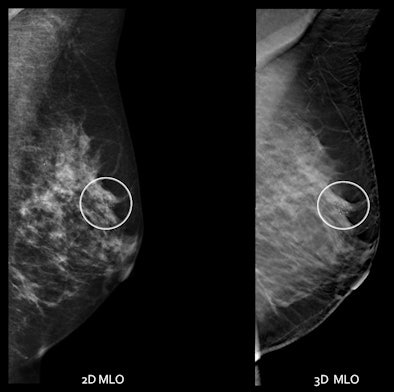 |
| Digital mammography and DBT, mediolateral oblique view. |
All patients underwent core biopsy, which identified 32 malignancies, seven atypical findings, and 64 benign lesions. Thirty-eight women have gone on to surgical excision, Destounis said. The average lesion size at surgical excision was 22 mm. Of these 38 who went to surgery, lesion size was available for 31 cases:
- DBT/digital mammography lesion sizes correlated to surgical size in 12 cases.
- Both digital mammography and DBT overestimated the lesion size in nine cases.
- Both underestimated the size in five cases.
- DBT correlated to surgical size better than digital mammography in five cases.
Now that the first DBT system has been approved by the U.S. Food and Drug Administration (FDA) (Selenia Dimensions 3D, Hologic), radiologists will begin to use it more, Destounis said. And it's important for radiologists to know that it's helpful for finding calcifications, not just masses.
"I really do think that DBT is here to stay," she said. "It's an adjunct to mammography that's a great way to get rid of overlap in images of women with dense breast tissue, or women who are at high risk."
| Mammography developer Hologic provided the DBT system used in the study. Destounis is a consultant with the company. |