Screening younger women for breast cancer catches tumors at an earlier stage and smaller size, and it also finds high-risk lesions in time for treatment, reducing a woman's subsequent risk, according to a study published in the May issue of the American Journal of Roentgenology.
Researchers at Case Western Reserve University wanted to assess the effects of the screening mammography recommendations released in 2009 by the U.S. Preventive Services Task Force (USPSTF). The task force at the time withdrew its previous recommendation that women between 40 and 49 be screened routinely, instead advising these women to consult with their physicians on whether to undergo screening.
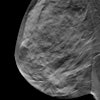
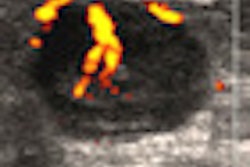
The researchers compared breast cancer stage at diagnosis in two groups of women between 40 and 49 years old: those undergoing screening mammography and those with a symptom needing diagnostic workup (AJR, May 2012, Vol. 198:5, pp. 1218-1222).
"The differences between the screened and unscreened groups in our study are provocative and suggest a real benefit from screening women ages 40 to 49 years," wrote lead author Dr. Mallory Kremer and colleagues.
Kremer's group examined the results of image-guided core-needle biopsies performed in women between the ages of 40 and 49 from January 2008 to December 2009. In patients diagnosed with breast cancer or a high-risk lesion, the team also tracked the reason for presentation, pathology, tumor size, stage, and receptor characteristics. The team used the chi-square test for statistical analysis.
Of 108 primary breast cancers, 71 were detected in the screened group and 37 in the unscreened group. Nearly half of the women diagnosed with breast cancer in the study received initial imaging at outside institutions; of these, 31% had full-field digital mammography (FFDM) and 65% had analog mammography. All mammography exams performed at Case Western were FFDM.
The researchers concluded the following:
- The screened group was significantly more likely to be diagnosed with ductal carcinoma in situ (DCIS) than the unscreened group (p = 0.001).
- Screened patients with invasive carcinoma were significantly more likely to be diagnosed at earlier stages (p = 0.025).
- The size of invasive breast tumors in the screened group was significantly smaller (p = 0.002).
- Of high-risk lesions, atypical ductal hyperplasia and lobular carcinoma in situ were most common.
- More screened patients were node-negative than unscreened patients (55% versus 39%, respectively).
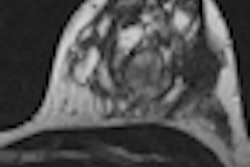
In an additional finding that would seem to support the efficacy of FFDM with dense breast tissue, of the screened group of 71 women, a subset of 17 were diagnosed with interval breast cancer, having had a BI-RADS category 1 or 2 mammography exam less than 12 months before cancer diagnosis, according to the authors. Sixteen of these 17 women had more than 50% density on mammography -- and had been imaged with analog devices at outside institutions.
The potential benefits of screening mammography programs are well-documented and contradict the USPSTF's recommendation, the group wrote. Furthermore, reducing the number of breast cancer deaths is not the only benefit of mammography.
"Standard treatment of higher-stage disease includes treatments with unwanted side effects, such as chemotherapy, mastectomy, node dissection, and chest wall radiation, each with attendant morbidity," Kremer and colleagues wrote. "Diagnosing breast cancer at the earliest stages reduces the likelihood of local and systemic recurrence and the need for additional toxic treatment."