It's been just over 30 days since California's version of breast density notification legislation went into effect. How is the law affecting clinical practice in the state's breast centers? Although they are complying, many breast imagers are skeptical of its value.
SB 1538 went into effect on April 1, making California the fifth state to implement a breast density notification law, after Connecticut, Texas, Virginia, and New York. As with the other laws, California's version requires women in the state to be notified following a mammogram if they have dense breast tissue.
The law may be in place, but California breast imagers and mammography experts aren't so sure it's the best way to deal with the issue of assessing a woman's breast density and cancer risk. AuntMinnie.com spoke with California radiologists about how they've implemented the legislation and what it could mean for screening mammography.
Grassroots efforts
The law in California and other states was sparked by the grassroots efforts of women who have received screening mammography, had cancers missed, and are now looking for a way to make breast cancer detection more effective.
But one problem with California's breast density notification law -- or any state's law, for that matter -- is that research studies on breast tissue density and cancer risk are a bit misleading, according to Dr. Haydee Ojeda-Fournier, medical director of the breast imaging section of Moores Cancer Center at the University of California, San Diego. The question of whether breast tissue density actually is a risk factor has not been resolved.
 Dr. Haydee Ojeda-Fournier from Moores Cancer Center.
Dr. Haydee Ojeda-Fournier from Moores Cancer Center.
"The existing studies compare breast cancer risk of patients who have fatty breast tissue to those women with extremely dense tissue," she told AuntMinnie.com. "But those two groups are extremes of each other. You have to look at data across all types of tissue density."
In fact, fewer than 10% of all women have "extremely dense" breast tissue, which is associated with twice the risk (relative risk of 2) of breast cancer as compared to women with average breast density. Some 40% of women have "heterogeneously dense" breast tissue, which is associated with a relative risk of approximately 1.2, according to Ojeda-Fournier.
"Breast density is just not a major cancer risk factor," she said.
What's more, California's breast density legislation raises three key issues, according to Ojeda-Fournier.
"The first drawback to this legislation that I see is that the government is legislating the way that we provide healthcare," Ojeda-Fournier told AuntMinnie.com. "And it's not yet clear whether breast density notification is appropriate or helpful or not."
A second concern is that breast imagers are telling patients with dense tissue that they're at higher risk for cancer, but they don't unequivocally know if that's true. This may cause some confusion and prompt some patients to conclude that mammography is no good at all.
Finally, there is a lack of alternative screening technologies to mammography. Ultrasound and MRI are available, and the data behind digital breast tomosynthesis are very good, "but no study has ever shown that screening ultrasound or MRI will save lives like we know mammography does," she said.
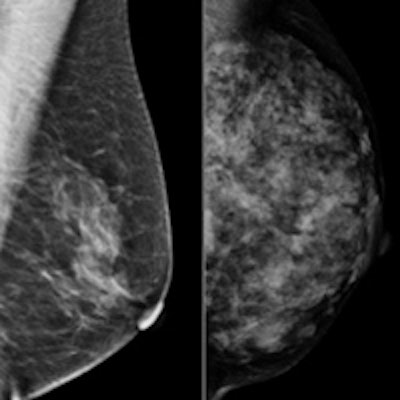
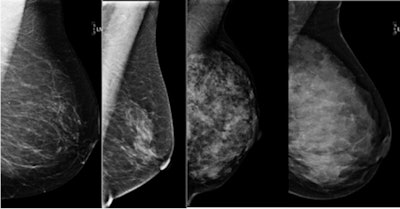 The four tissue types from left to right: almost entirely fat, scattered fibroglandular densities, heterogeneously dense, and extremely dense. The new California law applies to the last two, heterogeneously or extremely dense. Fewer than 10% of patients will have an extremely dense pattern. Image courtesy of Dr. Haydee Ojeda-Fournier.
The four tissue types from left to right: almost entirely fat, scattered fibroglandular densities, heterogeneously dense, and extremely dense. The new California law applies to the last two, heterogeneously or extremely dense. Fewer than 10% of patients will have an extremely dense pattern. Image courtesy of Dr. Haydee Ojeda-Fournier.Examples of implementation
Ojeda-Fournier's department began sending breast density notification letters before the law took effect on April 1. When a woman comes in for a screening mammogram, she completes an online risk assessment that is sent to one of the department's breast health specialists.
If the patient is at high risk for breast cancer and has dense tissue, the team recommends breast MRI in addition to mammography. In the past month, letters have gone out to more than half of patients seen for screening mammography -- but none have inquired, Ojeda-Fournier said.
 Dr. Grace Bhardwaj from Scripps Memorial Hospital Encinitas.
Dr. Grace Bhardwaj from Scripps Memorial Hospital Encinitas.
California's law has also not yet affected Valley Radiology Consultants of San Diego, according to president Dr. Allen Nalbandian: Since the law went into effect, the practice has sent out more than 3,000 breast density notification letters, but it has not heard back from either patients or referring physicians.
For the Imaging Center of Scripps Memorial Hospital Encinitas, compliance with the California law has gone fairly smoothly, according to Dr. Grace Bhardwaj, lead interpreting physician for mammography. Only one patient followed up in the month of April.
"We were concerned about how we were physically going to communicate information to our patients, in a redundant manner across our system," Bhardwaj told AuntMinnie.com. "It took some time to integrate IT and transcription."
Implementation aside, the law does raise some tricky issues, Bhardwaj said.
"Generally speaking, anything that raises awareness in patients about their healthcare options is a good thing," she said. "The downside to this legislation is that there's no medical standard right now -- we can suggest ancillary imaging to our patients with dense breast tissue, but there's no standard of care for how to work up various densities. From a medical standpoint, we have a better sense of how to do that with the genetic risk of cancer as opposed to breast tissue density."
Do the pros outweigh the cons?
Breast density is an important factor to consider when assessing a woman's breast cancer risk, but it needs to be considered in context, Nalbandian told AuntMinnie.com.
 Dr. Allen Nalbandian from Valley Radiology Consultants of San Diego.
Dr. Allen Nalbandian from Valley Radiology Consultants of San Diego.
"Even though I think breast density is an important consideration, like many other things in medicine, the politics and the nonscientific considerations are a bit ahead of the science," he said. "Our angle is that density for a particular patient should be evaluated in context of other breast cancer risk factors."
If anything, California's breast density notification law will serve as a starting point to a conversation about tailored breast cancer screening and further development and testing of breast imaging technology, Nalbandian said.
"The breast density issue serves as an important segue into a conversation between patients and doctors about tailored screening, a trend that will further mature as we go along," he said. "And we're also diversifying our screening armamentarium, as mammography continues to evolve. We'll see further penetration of digital breast tomosynthesis, breast MRI -- which is the current gold standard for screening high-risk patients -- and whole-breast ultrasound. The medical community is developing tools that we'll be able to apply in different contexts depending on the particular patient and the risk that she carries."
Be prepared
 Bonnie Rush from Breast Imaging Specialists.
Bonnie Rush from Breast Imaging Specialists.
Regardless of whether or not they operate in a state with a density law, breast imagers need to offer supplementary imaging if they want to maintain market share, according to Bonnie Rush, consultant and president of Breast Imaging Specialists of San Diego.
"Breast imaging centers can choose to ignore it if they're in a state that doesn't have a law, but women are educating themselves on this issue and looking around to see who is offering breast imaging other than mammography," Rush told AuntMinnie.com.
She advises breast imaging centers to be technology leaders in their areas: the most proactive center for early detection for women in their community.
"Women are in the driver's seat on this one, and breast imagers have got to listen to what's happening in their communities and plan ahead," she said.




















