Adding digital breast tomosynthesis to mammography significantly increases image interpretation time, which begs the question of how using the technologies together affects clinical efficiency, according to a new study published in the January issue of Radiology.
Researchers from Massachusetts General Hospital compared interpretation times for conventional screening mammography and combined tomosynthesis and mammography; they found that adding tomosynthesis increased the amount of time required to interpret a case by 47% (Radiology, January 2014, Vol. 270:1, pp. 49-56).
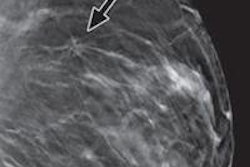
Several recent studies have reported the benefits of combined tomosynthesis and mammography over conventional digital mammography alone, including improved performance and diagnostic accuracy, reduced recall rates, and higher cancer detection rates. In light of these benefits, many centers are combining tomosynthesis and mammography for screening and diagnostic applications.
But how does this combination play out in clinical practice? It's been unclear, according to lead author Dr. Pragya Dang and colleagues.
"To our knowledge, [no study has] prospectively evaluated the real-world effect of the addition of tomosynthesis to mammography on image interpretation times as a part of normal clinical screening practice," the group wrote. "The purpose of our study was to determine the effect of implementing a screening tomosynthesis program on real-world clinical performance."
For the study, Dang and colleagues invited 10 radiologists to read images from cases in which screening digital mammography was used alone or screening mammography was combined with tomosynthesis. The radiologists read images from 3,665 examinations (1,502 tomosynthesis and mammography cases and 2,163 digital mammography studies) from July 2012 to January 2013. Dang's team recorded the number of cases reported per hour, per radiologist.
The mean number of studies interpreted per hour was 24 for combined tomosynthesis and mammography, compared with 34 for digital mammography alone. A mean of 10 fewer studies were interpreted per hour for combined tomosynthesis and mammography, the researchers found.
Mean interpretation time was 2.8 minutes for combined tomosynthesis and mammography and 1.9 minutes for digital mammography, according to the authors. Interpretation time with tomosynthesis and mammography was 47% longer than with digital mammography alone.
Experience correlated with shorter reading times, Dang and colleagues noted. Radiologists with more breast imaging experience required less additional time overall to read images from combined tomosynthesis and mammography examinations.
Breast imaging centers may decide that the increased reading time is acceptable, given the benefits of the combination. But it's important to have the facts, the authors concluded.
"This estimation of the differential interpretation time should prove extremely useful in preparing for the effect on radiologists' workload and in planning for staffing requirements and resource allocation as this technology is implemented," they wrote.