A new study published in the February issue of Radiology found that breast MR is useful for working up suspicious lesions classified as BI-RADS 4 at mammography or ultrasound -- and, in fact, can help avoid 92% of unnecessary biopsies.
The BI-RADS 4 category classifies lesions as suspicious and recommends that biopsy be considered. But the average positive predictive value of mammography and ultrasound is low, with mammography ranging from 18.4% to 31% and ultrasound from 6.7% to 13.2%, which can result in unnecessary biopsies. Because breast MR's diagnostic accuracy has continued to increase over the past decade, researchers from University Hospital Aachen in Germany investigated whether the technology could help work up these suspicious lesions.
"The reservations against the use of MR imaging for problem-solving were shaped during a time when breast MR imaging was still evolving and the radiologic community was still learning how to appropriately image the breast ... and how to interpret the respective findings," wrote lead author Dr. Kevin Strobel, PhD, and colleagues. However, growing expertise in breast MRI "has greatly improved our understanding of the natural appearance of the breast and the MR imaging manifestations of benign and malignant changes."
The study included 340 women with 353 lesions that were found at screening mammography (198) or ultrasound (155). The lesions were rated BI-RADS category 4 after appropriate conventional workup between June 2010 and January 2013. All of the women underwent standard dynamic contrast-enhanced MR imaging (Radiology, February 2015, Vol. 274:2, pp. 343-351).
Of the 353 lesions, 66 (18.7%) were true-positive (23 cases of ductal carcinoma in situ and 43 invasive cancers) and 287 (81.3%) were false-positive. MR showed no breast cancer in 92% of the false-positive findings (264 of 287) and helped confirm the presence of breast cancer in 63 of 66 malignancies, according to the authors.
Among the 198 mammography findings, 71 were masses, 34 were asymmetric densities, 15 were architectural distortions, and 78 were clustered microcalcifications. Of the 155 ultrasound findings, 115 were masses and 40 were nonmass lesions.
Breast MR identified all mammographic findings of invasive cancer and 18 of 21 mammographic findings that showed ductal carcinoma in situ (DCIS). It identified all 18 ultrasound findings that were invasive breast cancer and two that were pure DCIS, Strobel and colleagues found.
MRI had a relatively high false-negative rate for DCIS found on mammography, at 12%; the three false-negative cases were low-grade, at 6 mm, 7 mm, and 11 mm. On the other hand, breast MR found additional invasive cancers in three women with false-positive findings from mammography and ultrasound.
As for mammographic findings other than microcalcifications, MRI increased the positive predictive value (PPV) from 17.5% to 78%, with a false-negative rate of zero. For all ultrasound findings, MRI increased PPV from 12.9% to 69%, again with a false-negative rate of zero. MRI resulted in false-positive findings that led to MRI-guided biopsy in five of the 340 patients (1.5%).
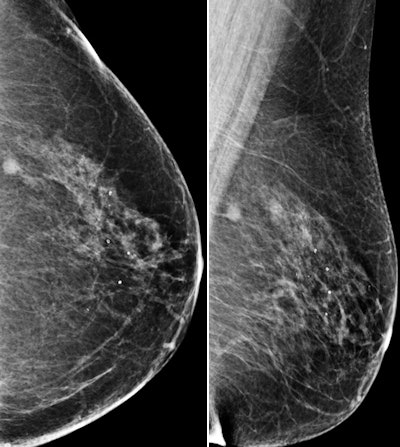 Images are of a 69-year-old postmenopausal woman who had mammographic screening. Screening mammograms (left craniocaudal and left mediolateral oblique views, respectively) show a mass with ill-defined margins in the posterior third of the left breast at 1 o'clock position. All images courtesy of RSNA.
Images are of a 69-year-old postmenopausal woman who had mammographic screening. Screening mammograms (left craniocaudal and left mediolateral oblique views, respectively) show a mass with ill-defined margins in the posterior third of the left breast at 1 o'clock position. All images courtesy of RSNA.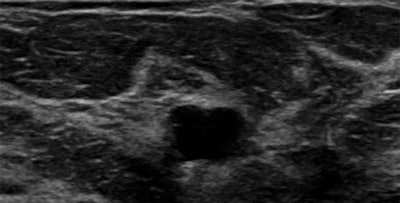 B-mode ultrasound scan shows hypoechoic mass with ill-defined margins in left breast at 1 o'clock position.
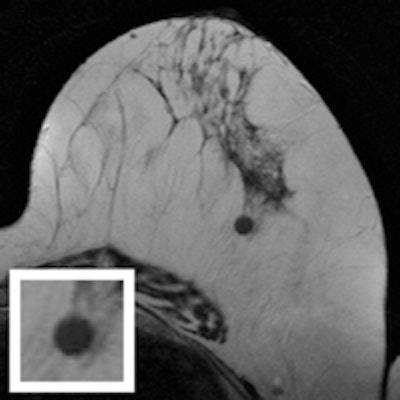
B-mode ultrasound scan shows hypoechoic mass with ill-defined margins in left breast at 1 o'clock position.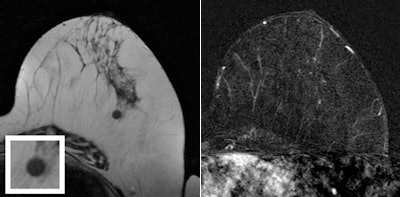 T2-weighted turbo spin-echo MR image and magnification view (left) show a round mass as the correlate of the mammographic finding at 1 o'clock in the left breast. The mass is isointense with discrete internal septations. Subtracted T1-weighted gradient-echo MR image (right) obtained after administration of contrast shows no enhancement of the lesion. Ultrasound-guided core needle biopsy was performed, and histologic examination showed a sclerosed fibroadenoma.
T2-weighted turbo spin-echo MR image and magnification view (left) show a round mass as the correlate of the mammographic finding at 1 o'clock in the left breast. The mass is isointense with discrete internal septations. Subtracted T1-weighted gradient-echo MR image (right) obtained after administration of contrast shows no enhancement of the lesion. Ultrasound-guided core needle biopsy was performed, and histologic examination showed a sclerosed fibroadenoma.Proceed with caution?
The technology's relatively high false-negative rate for pure clustered microcalcifications suggests that radiologists should proceed with caution when confronted with negative MR results in these cases, according to Strobel and colleagues.
However, that doesn't mean that breast MRI is worthless in women with BI-RADS 4 microcalcifications, they noted. In 45 of 78 women with pure clustered microcalcifications, MRI could have been used to avoid vacuum biopsy. And in 22 women with positive MRI results for DCIS, the technology helped clinicians upgrade the mammographic finding to BI-RADS 5.
"For the time being, MR imaging cannot be used to discourage biopsy in women with pure clustered calcifications," the group concluded. "However, we expect that with increasing understanding of the predictive implications of the MR imaging phenotype of DCIS, this will probably change."