The number of primary care physicians who would recommend screening mammography to women in their 40s plummeted after they received information in a "teaching session" about the "harms" of screening, according to a study published in the Journal of Multidisciplinary Healthcare.
Initially, more than 82% of primary care physicians and nurses said they would recommend screening mammography to women in their 40s, researchers from the University of Alabama at Birmingham reported. But that number fell to less than 9% after doctors and nurses received what the researchers called a teaching session, using content based on the breast screening criteria issued in 2009 by the U.S. Preventive Services Task Force (USPSTF). USPSTF at that time withdrew the group's previous stance recommending screening for women in their 40s.
A prominent breast imaging radiologist thinks the study's findings could represent a growing disconnect between primary care physicians and radiologists regarding the value of breast screening for women in their 40s -- a gulf that could result in some women not getting breast screening when it could save their lives.
USPSTF fallout
It's been six years since USPSTF recommended that women ages 40 to 49 be counseled about the risks and benefits of breast screening, rather than sent directly to mammography, wrote the research team led by Dr. Teresa Bryan, a general internist. But few providers adhere to this recommendation in practice, according to the authors.
"Women indicate that they desire to be actively involved in decision-making regarding medical testing related to breast health," they wrote. "However, research has shown that providers do not typically include women in decision-making about screening."
As a result, Bryan's group wanted to assess the knowledge, attitudes, and comfort level of primary care providers in counseling women about breast cancer screening through a study conducted from June to September 2012. The study consisted of anonymous questionnaires given before and after 30-minute "educational interventions" (J Multidiscip Healthc, May 2015, Vol. 2015:8, pp. 209-216).
The session featured information on USPSTF's 2009 breast cancer screening guidelines, which are ostensibly the standards used by the U.S. Department of Veterans Affairs (VA). It also included information on the benefits and harms of mammography screening, risk assessment tools, and counseling methods. Session participants were given material regarding breast cancer screening decisions for average-risk women in their 40s through a discussion guide developed by the VA's National Center for Health Promotion and Disease Prevention.
The intervention reached 87 out of 121 staff members. Bryan and colleagues held 13 teaching sessions, with an average of seven attendees at each. A total of 165 surveys (78 before the intervention and 87 after the intervention) were received, for a pretraining response rate of 90% and a post-training rate of 100%.
Increased willingness?
The educational session increased the willingness of providers to talk with patients about breast cancer screening -- especially about its harms. The percentage of participants who said they would discuss the patient's screening preferences before making a recommendation increased from 5.3% before the intervention to 53.1% after it, and attitudes favoring the discussion of the harms of mammography increased dramatically pre- and postintervention, from 33.8% to 90.5%.
But the intervention also dramatically reduced the inclination of providers to recommend screening for women between the ages of 40 and 49. Before the session, 82.4% of participants said they would recommend that all women in this age group be screened; after the session, 8.6% said they would make that recommendation. Also, before the educational intervention, 12.3% of participants said they would advise patients to wait until age 50 to begin screening, while after the session, 38.3% said they would give this advice.
Dealing with disconnect
The study indicates that there could be a widening disconnect between primary care physicians and radiologists in their understanding of the worth of breast cancer screening. This situation could be a big problem, according to Dr. Stamatia Destounis of Elizabeth Wende Breast Care in Rochester, NY.
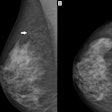
"Risk assessment and counseling specific to individual women is extremely important and very helpful for high-risk patients. But the fact is that most women diagnosed with breast cancer are not considered high risk," she told AuntMinnie.com via email. "Radiologists can explain to our fellow healthcare providers the benefits of identifying breast cancer early -- before it is found on breast examination."
It's all well and good to discuss both benefits and harms, but the conversation needs to provide context, Destounis cautioned.
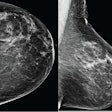
"Many women in the 40- to 49-year-old range have dense breast tissue, and simply stating that they don't need any screening until age 50 does them a disservice," she said. "Healthcare providers need to put the fears and anxiety associated with false-positive callbacks in perspective, so that women can make truly informed choices."