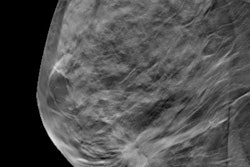
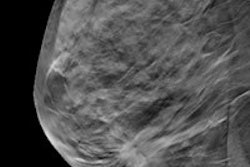
Digital breast tomosynthesis (DBT) finds 54% more cancers than 2D mammography and reduces recall rates by almost 20%, according to a new study published in Radiology. Even better, the technology identifies lesions in dense breast tissue, which mammography tends to miss.
So could DBT become the primary screening modality for breast cancer? It sure seems like it, lead author Dr. Richard Sharpe from Beth Israel Deaconess Medical Center in Boston told AuntMinnie.com.
"As the technology matures, we predict that more practices will put strategic plans into place to install DBT and use it as their sole breast cancer screening modality," Sharpe said.
 Dr. Richard Sharpe of Beth Israel Deaconess Medical Center.
Dr. Richard Sharpe of Beth Israel Deaconess Medical Center.Furthermore, finding cancer earlier and reducing the number of follow-up imaging exams, false positives, and biopsies would be good not only for women, but also for overall healthcare costs, the authors wrote.
Radical results
Sharpe and colleagues conducted the study -- which was funded by Beth Israel alone, with no industry support -- because of the results they were seeing after DBT was incorporated into the department in 2012.
"When we first acquired the tomosynthesis equipment, we immediately had the feeling that we weren't recalling as many patients," Sharpe said. "So we started to look into the cancer detection and recall rates of the two modalities, and found that with DBT, not only were we calling fewer patients back, but we were detecting more cancers."
The study included a large cohort of 85,852 women who presented for breast cancer screening at Beth Israel between 2011 and 2014. After the DBT device was introduced into the screening program, women were assigned to the first available machine, whether it was the DBT unit or a 2D mammography unit.
Of the total number of exams in the study, 5,703 were DBT and 80,149 were 2D mammography. For each modality, Sharpe's group calculated overall cancer detection and recall rates, as well as recall rates according to patient age and breast density (Radiology, October 9, 2015).
Conventional mammography found 280 cancers out of 85,852 mammography exams, for a detection rate of 3.5 per 1,000 women. DBT found 31 cancers out of 5,703 DBT exams, for a rate of 5.4 per 1,000 women -- an increase of 54.3% over 2D mammography.
As for recalls, the overall rate was 6.1% for DBT and 7.5% for 2D mammography, a difference of 19%, the group found. DBT's recall rates were lower compared to mammography across all breast tissue density types, but the differences were statistically significant in heterogeneously and extremely dense tissue -- types of tissue that can make mammography less effective. DBT's recall rates were also statistically significant compared to mammography in the 40-to-49 and 60-to-69 age groups. And DBT dramatically improved recall rates in women who were undergoing their first breast cancer screening exam.
| DBT vs. 2D mammography for screening | ||||
| DBT | 2D mammography | p-value | Recall rate reduction | |
| Overall | 6.1% | 7.5% | < 0.0001 | 19% |
| For women 40-49 | 8.7% | 10.9% | 0.0075 | 21% |
| For women 60-69 | 3.7% | 5.9% | 0.0006 | 17% |
| Heterogeneously dense tissue | 7.3% | 9.3% | 0.0048 | 21% |
| Extremely dense tissue | 4.7% | 6.5% | 0.0429 | 27% |
| Undergoing screening for 1st time as baseline | 9.9% | 19.6% | < 0.0001 | 50% |
"Recalling significantly fewer patients after screening has many benefits," Sharpe and colleagues wrote. "Patients not recalled after screening may benefit by experiencing fewer missed days of work, less anxiety, fewer additional imaging evaluations, fewer unnecessary biopsies, and decreased healthcare and transportation costs."
What's next?
Future research could address whether using DBT for screening would result in those particular benefits, according to the researchers. But in any case, using the technology alone for screening is definitely in the near future, Sharpe told AuntMinnie.com.
"Our findings reinforce the validity of using tomosynthesis alone for screening," he said. "We hope these results will encourage practices to adopt the technology into their screening programs."