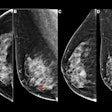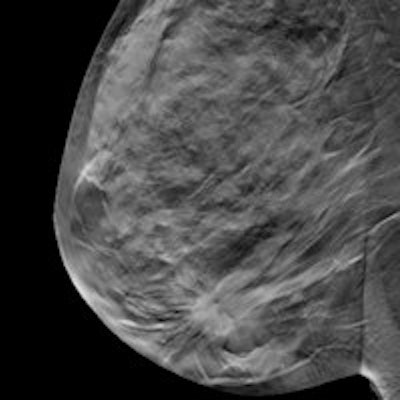
A new literature review published in The Breast has confirmed that adding digital breast tomosynthesis (DBT) to breast screening with full-field digital mammography (FFDM) boosts invasive cancer detection rates, and it may reduce recall and false-positive rates as well.
While evidence has suggested that DBT performs better than FFDM for diagnostic applications, the relative performance of DBT and FFDM for finding cancer in a screening population has not been fully explored, researchers from both Europe and the U.S. wrote. One of the strengths of this review was the extent of the data that it included, corresponding author Julie Glanville of the University of York in the U.K. told AuntMinnie.com via email.
"It was unusual for us to be reviewing data which are so extensive and consistent in supporting the use of breast tomosynthesis," she said. "Very often we are analyzing one or two small studies and it is difficult to draw conclusions, but that was not the case with this review. As far as we are aware, this is the first systematic review of tomosynthesis to be published."
Stateside and across the pond
In October 2014, Glanville and colleagues identified five studies that compared the combination of DBT plus FFDM to FFDM alone for breast screening. Two were from Europe:
- Skaane, 2013 (12,631 exams) -- the Oslo Tomosynthesis Screening Trial (OTST) in Norway
- Ciatto, 2013 (7,292 women) -- the Screening With Tomosynthesis or Standard Mammography (STORM) trial in Italy
The remaining trials were conducted in the U.S.:
- Destounis, 2014 (524 women)
- Friedewald, 2014 (454,850 exams)
- Lourenco, 2014 (25,498 exams)
The studies reported relative cancer detection, as well as false-positive and recall rates for each screening protocol. Glanville and colleagues analyzed the results of the European and U.S. studies separately due to differences in breast cancer rates, demographics, and screening practices (The Breast, March 25, 2016).
For the combination of DBT and FFDM, the European studies found a higher overall cancer detection rate that was statistically significant, as well as a higher invasive cancer detection rate (p < 0.001). These studies did not show a statistically significant difference in the detection rate for noninvasive cancers, however.
Although the cancer detection results were similar for the U.S. studies, the increase in detection rate for all cancers and invasive cancers was less than in the European studies, due perhaps to the shorter screening interval in the U.S. compared to Europe (one year versus two years). Other contributing factors could be the use of double reading in the European trials, or the relatively older age of women who participate in European screening programs.
| Breast cancer screening rates | ||||
| Study | False-positive rate | Recall rate | Cancer detection rate | Invasive cancer detection rate |
| DBT + FFDM | ||||
| STORM | 3.5% | 4.3% | 0.81% | 0.71% |
| OTST: single reading | 5.3% | 2.8% | 0.8% | 0.64% |
| OTST: double reading | 8.5% | 3.7% | 0.94% | 0.74% |
| Destounis | 3.6% | 4.2% | 0.57% | 0.19% |
| Lourenco | 5.9% | 6.4% | 0.46% | 0.23% |
| Friedewald | 8.4% | 8.9% | 0.55% | 0.41% |
| FFDM | ||||
| STORM | 4.4% | 5% | 0.53% | 0.48% |
| OTST: single reading | 6.1% | 2.1% | 0.61% | 0.44% |
| OTST: double reading | 10.3% | 2.9% | 0.71% | 0.53% |
| Destounis | 11.1% | 11.4% | 0.38% | 0.19% |
| Lourenco | 8.8% | 9.3% | 0.54% | 0.33% |
| Friedewald | 10.1% | 10.6% | 0.43% | 0.29% |
Next steps?
Data on interval cancers found with DBT are still lacking, Glanville and colleagues wrote. But the evidence gathered in this review suggests that cancer detection rates and invasive cancer detection rates are higher when DBT is used with FFDM than when FFDM is used alone. This may mean that adding the technology to screening programs could find cancers earlier and thus reduce morbidity and mortality.
"[These studies] show that DBT plus FFDM, compared to FFDM, yields higher invasive cancer detection rates, increasing the effectiveness of breast cancer screening," the group wrote. "The use of DBT may reduce recalls and thereby reduce both program costs and distress caused by a false-negative recall."
How might the team's review affect the use of DBT? It could boost reimbursement, Glanville told AuntMinnie.com.
"Clinical guidelines and payment policies influence the adoption of any new procedure," she said. "As such, this systematic review should be helpful when guideline panels and payors update their evidence reviews for tomosynthesis."
Finally, when the researchers conducted this analysis, there were limited follow-up data published about women screened with tomosynthesis. That has now changed, according to Glanville.
"Since the review was conducted, several studies have published follow-up data," she said. "These studies, along with other emerging evidence, may warrant an update review in the future which will provide even richer information."