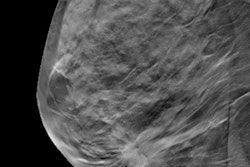
CHICAGO - It seems like a good idea: When using digital breast tomosynthesis (DBT), synthesize the 2D mammography images from the tomosynthesis data to reduce radiation dose. But are these images really good enough to replace actual 2D mammography? Researchers addressed this question on Tuesday morning at RSNA 2015.
 Martin Yaffe, PhD, from the University of Toronto.
Martin Yaffe, PhD, from the University of Toronto.In an overall orientation to DBT technology, Martin Yaffe, PhD, of the University of Toronto, cautioned that synthesized 2D images aren't quite ready for prime time.
"These images still have a way to go until radiologists consider them good enough to be a true replacement for 2D mammography," he said.
However, clinical studies presented at the session painted a different story, suggesting that synthesized 2D images may be equal to or better than conventional 2D images when used with tomosynthesis -- not only for identifying particular types of lesions, but also in terms of recall rates. And using synthetic images reduces radiation dose by 45%, one group found: DBT plus conventional 2D carries a dose of 3.53 mGy per view, while DBT with synthetic 2D images carries a dose of 1.95 mGy per view, just over mammography's 1.58 mGy per view.
Synthetic images match conventional
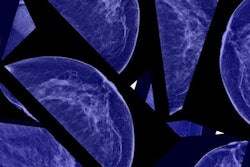
Yale researchers found that synthetic 2D images used in combination with digital breast tomosynthesis are equal to -- or even better than -- conventional 2D images plus tomosynthesis.
Dr. Melissa Durand and colleagues included 201 screening mammograms that had been performed between August 2014 and January 2015 with both synthetic and conventional 2D mammography plus tomosynthesis.
 Dr. Melissa Durand from Yale University.
Dr. Melissa Durand from Yale University.The team assessed calcifications, asymmetries, masses, and architectural distortions, categorizing the synthesized images as better, equally visualized, or less well-visualized than the 2D mammography images. Five readers first interpreted synthesized 2D plus tomosynthesis exams, followed by conventional 2D plus tomosynthesis exams.
In the study sample, there were 102 calcifications (50.8%), 58 asymmetries (28.9%), 29 masses (14.4%), and 12 architectural distortions (6%). Forty-six percent of the images showed dense tissue.
The majority of these findings, or 82%, were equally or better seen with synthesized 2D images plus tomosynthesis -- especially architectural distortions and calcifications. Durand and colleagues found that neither density nor age significantly affected the visibility of the findings. Recall rates did not differ significantly, with a rate of 10.9% for the synthesized images and a rate of 9.5% for the 2D images. The cancer detection rate was the same.
Durand acknowledged that 18% of the findings were less well-seen with the combination of synthetic 2D and tomosynthesis, compared with conventional 2D plus DBT. But no cancers were missed, she said.
"Using synthetic 2D plus DBT for screening has the potential to provide the advantages of tomosynthesis without the extra radiation," she concluded.
What about recall rates?
In another presentation, Dr. Samantha Zuckerman from the University of Pennsylvania Health System reported that using synthesized 2D mammography images with digital breast tomosynthesis yields recall rates comparable to those of conventional mammography in combination with DBT.
"At U. Penn, we're now in our fifth year of screening all patients with DBT," she told session attendees. "We implemented synthetic 2D in September 2014, and in January of this year began using it for all screening."
Zuckerman and colleagues compared recall rates generated with synthetic 2D plus DBT and conventional mammography plus DBT, and analyzed the types of lesions that were recalled. Between October 2011 and February 2013, 15,571 women were screened with the digital mammography-DBT combination. Meanwhile, 2,090 women were screened with the synthetic 2D-DBT combination between January and March 2015.
The overall recall rate for synthetic 2D plus DBT was 7.1%, compared with 8.8% for mammography plus DBT, the researchers found. The two combinations were comparable in terms of the type of lesion recalled, although synthetic 2D plus DBT had a significantly lower recall rate for focal asymmetries when compared with conventional 2D and DBT (3.2% versus 4.5%).
"Synthetic 2D is an acceptable replacement to digital mammography in breast cancer screening with tomosynthesis, offering decreased dose and recall rates and similar cancer detection rates," Zuckerman said.