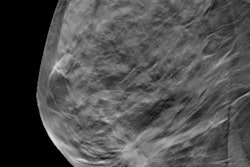
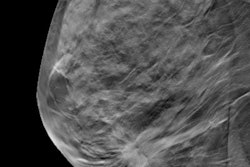
Adding screening digital breast tomosynthesis (DBT) to annual mammography is cost-effective when compared with mammography alone -- particularly in women between the ages of 40 and 49, according to a new study published online August 22 in the American Journal of Roentgenology.
The findings are good news as the push toward value-based healthcare continues, researchers from Yale University wrote. For a screening test to be considered cost-effective, it must have high sensitivity and adequate specificity and improve patient outcomes at a cost below societally defined thresholds (that is, society's willingness to pay for healthcare services), according to lead author Dr. Vivek Kalra and colleagues.
Tomosynthesis fits the bill, Kalra told AuntMinnie.com.
"We found that adding annual tomosynthesis to 2D mammography is cost-effective across all ages and breast densities, but particularly in the 40-to-49 age group," he said.
Quality of life
Kalra's team designed a model for annual screening with both tomosynthesis and 2D mammography for a population of women ages 40 to 74 across all breast tissue densities. The group defined model parameters from a multi-institutional study of more than 450,000 patients, institutional data from 13,000 patients, a literature review, and Medicare reimbursement rates. The base case for the model was a 56-year-old woman presenting for an annual screening exam (AJR, August 22, 2016).
 Dr. Vivek Kalra from Yale University.
Dr. Vivek Kalra from Yale University.The researchers determined thresholds for DBT's net monetary benefit from a reduction in recall rates between tomosynthesis and 2D mammography alone. They used a standard "willingness to pay" threshold of $100,000 per quality-adjusted life year (QALY) for their analysis. The model also analyzed the incremental cost-effectiveness ratio (ICER) of tomosynthesis (ICER reflects the cost of one strategy to achieve a full quality-adjusted life year compared with another strategy and is calculated by dividing the cost of each strategy divided by their expected utility).
In the group's base case analysis, annual tomosynthesis increased the QALY measure from 15.46 for 2D mammography alone to 15.50 for tomosynthesis. This improvement came at a cost increase of only around $800; annual tomosynthesis screening cost $15,312, while 2D mammography cost $14,500.
Kalra and colleagues also calculated incremental net monetary benefit (NMB), which translates into dollars the net gain of incremental benefits against the increased costs based on the willingness-to-pay threshold. Differences between the modalities had an overall incremental NMB of $3,188 and an overall incremental cost-effectiveness ratio of $20,300 per QALY. When the researchers broke down the results by age group, the incremental NMB for women 40 to 49 was three times more than the NMB for women 50 to 59.
"Three times greater NMBs in women 40 to 49 years old compared to those seen in women 50 to 59 years old may warrant re-evaluation of mammography screening recommendations," the team concluded.
Good enough?
But in a commentary on the study, published online August 17, a group led by Dr. Christoph Lee from the University of Washington criticized the study model, suggesting that it falls short in three ways in which models are measured for quality: structure, including the underlying assumptions used to create the model; the robustness of the data used; and model validation.
"In all three areas, the methods and approach described by Kalra et al do not meet criteria for a rigorous model, making their results insufficient for confirming that annual combined screening is truly cost-effective," Lee and colleagues wrote. They "present a shallow model that uses observable outcomes (e.g., improved cancer detection rates) but does not specify processes that lead to those outcomes."
Tomosynthesis may show promise for the early detection of breast cancer, but its cost-effectiveness remains unclear, they wrote.
"More representative longitudinal outcomes data and simulation modeling, including the biennial screening strategies recommended by the U.S. Preventive Services Task Force and the American Cancer Society, are needed before the cost-effectiveness of tomosynthesis screening can be established," they concluded.