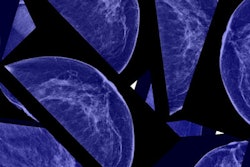
The U.S. Patient Protection and Affordable Care Act (ACA) has increased adherence to mammography screening by eliminating out-of-pocket costs, according to a new study published January 9 in Cancer. At the same time, reducing expenses did not increase colonoscopy rates among poorer patients.
The results are relevant as researchers and public health officials try to predict how patients will fare in the likely event that the incoming Trump administration and Congress act to eliminate the insurance program.
The ACA, signed into law in 2010 and implemented in 2011, aimed to cover individuals who were previously uninsured or underinsured. One goal of the ACA was to eliminate out-of-pocket expenditures for preventive services such as mammography and colonoscopy, potentially increasing compliance with guidelines by eliminating financial barriers to screening.
In their study, researchers from University Hospitals Cleveland Medical Center and Case Comprehensive Cancer Center in Cleveland looked at Medicare claims data to determine any changes in the use of mammography and colonoscopy among Medicare beneficiaries before and after implementation of the Affordable Care Act (Cancer, January 9, 2016).
They identified women ages 70 and older who had not undergone mammography in the previous two years, and both men and women ages 70 and older without colonoscopy in the past five years. The researchers also identified patients who were screened in the two years prior to ACA implementation (2009 and 2010) and during the two years after implementation (2011 and 2012).
In all, the sample included 862,267 women for the mammography analysis, and results were divided by quartile to show the impact of the ACA on individuals of different socioeconomic status and income. A lower socioeconomic status was associated with less screening uptake, but the disparities were smaller during the ACA period, compared with before it was implemented (p < 0.001).
For example, the odds ratio that someone in the lowest quartile of income would experience mammography screening, compared with someone in the highest income quartile, increased from 0.87 before the ACA to 0.94 after implementation. With respect to education, the odds ratio for the lowest quartile went from 0.76 to 0.86.
Regarding colonoscopy, on the other hand, the researchers found that screening uptake both before the ACA and after implementation was based on education level and to some extent income. However, there were no significant changes in colonoscopy and socioeconomic status before and after ACA implementation. In comparison with the highest quartile, the odds ratio for the lowest quartile was 0.94 before the ACA and 0.92 after implementation for income, and 0.96 before the ACA and 1.00 after implementation for education level.
Study limitations included a lack of clinical detail that could not distinguish between screening and diagnostic indications. Also, the study did not include enrollees in Medicare Advantage or Medigap plans, and it was limited to an older population of mostly Caucasian patients.
"The findings support the removal of out-of-pocket expenditures as a barrier to the receipt of recommended preventive services but emphasize that for colonoscopy, other factors such as a fear of sedation, perceived discomfort, and a need for bowel preparation should be considered," concluded lead author Dr. Gregory Cooper and colleagues. "We suggest that future studies examine the ACA's impact in other populations, including newly insured individuals."