Can software that calculates breast density perform as well as a radiologist and help identify a woman's future risk of breast cancer -- in particular, the risk of invasive interval cancers? Yes, it can, according to research published May 1 in the Annals of Internal Medicine.
After conducting a large case-control study, a multi-institutional team of researchers led by Dr. Karla Kerlikowske of the University of California, San Francisco (UCSF) concluded that automated and clinical breast density assessment methods yielded comparable results for predicting the risk of cancer detected in subsequent mammography screening and, in particular, the risk of interval cancer.
"Automated measures have the advantage of being more reproducible than clinical measures, so given [that] automated and clinical breast density assessment methods were equally accurate at predicting screen-detected and interval cancer, automated measures may be favored since they are more reliable," Kerlikowske told AuntMinnie.com.
Subjectivity, reproducibility issues
Breast density contributes to the development of 30% of breast cancers, and it is one of the strongest risk factors for breast cancer, according to Kerlikowske. But there are concerns over the subjectivity and reproducibility of clinical breast density measurements -- classified subjectively by radiologists into BI-RADS density categories -- particularly as they are used as part of breast cancer prevention strategies.
Variation in clinical BI-RADS density interpretations within and across radiologists has clinical implications; reporting of breast density may guide screening frequency, can lead to recommendations for supplemental imaging beyond screening mammography, and can affect risk assessment with risk-prediction models such as the Breast Cancer Surveillance Consortium (BCSC) risk calculator and Tyrer-Cuzick breast cancer risk evaluation tool.
"Thus, we wanted to know if an automated measure of breast density could similarly predict screen risk of cancer detected through mammography screening and the risk of interval invasive cancer -- that is, cancer diagnosed within a year of a negative mammography result that is found on clinical examination," she said. "If the automated and clinical BI-RADS measures are similar in prediction but automated [is] more reproducible, then automated measures could be used for recommendations for supplemental imaging, risk assessment, and to guide screening frequency."
Case-control study
The researchers performed a case-control study involving patients from the San Francisco Mammography Registry and a screening cohort from the Mayo Clinic in Rochester, MN. They compared 1,609 participants who had screening-detected cancer and 351 patients who had interval invasive cancer with 4,409 matched control participants who did not have previous breast cancer or breast implants. All control participants had at least one normal screening mammogram on or after the date that their matched participant case had been diagnosed with cancer.
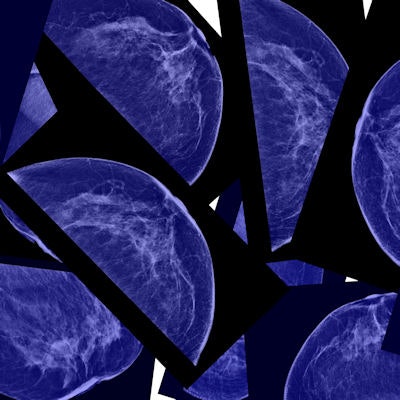
As part of routine clinical practice during mammography interpretation, radiologists classified breast density using the BI-RADS density categories: A (almost entirely fatty), B (scattered fibroglandular densities), C (heterogeneously dense), and D (extremely dense). Automated breast density measurements were performed on version 1.53 of the Volpara breast density assessment software (Volpara Solutions). Volumetric percentage density (VPD) was calculated by dividing the software's calculation of dense breast volume by total breast volume and then multiplying by 100. Four categories analogous to BI-RADS categories were then determined: A (VPD less than 4.5%), B (4.5% to 7.49%), C (7.5% to 15.49%), and D (15.5% or greater).
Of the women whose breast density had been categorized by automated BI-RADS assessment six months to five years before diagnosis, those with extremely dense breasts had a 5.65-fold higher risk of interval cancer and a 1.43-fold higher risk for screening-detected cancer than those with scattered fibroglandular densities, according to the authors. This difference was statistically significant (p < 0.001). Clinical density assessment had similar statistically significant differences for the association between breast density and interval cancers versus screening-detected cancers.
The two measurements offered similar discriminatory accuracy -- as determined via the area under the curve from receiver operating characteristic (ROC) analysis -- and both were better at predicting the risk for interval cancers than they were for screening-detected cancers. The differences in performance between the two methods were not statistically significant.
| Automated software vs. clinical assessment for predicting future breast cancer | ||
| Clinical density assessment | Automated density assessment | |
| Interval cancers | 0.72* | 0.70 |
| Screening-detected cancers | 0.62 | 0.62 |
"This finding suggests that either automated or clinical BI-RADS measures could be used to inform women of their breast density and associated interval and screen-detected cancer risk," the authors wrote.
The researchers also noted that similar associations with interval and screening-detected cancers were maintained by both automated and clinical BI-RADS assessment regardless of whether density was measured more than six months to less than two years before diagnosis or two to five years before diagnosis.
Implications for risk models
The study results have implications for breast cancer risk models, particularly those that predict the risk of the more aggressive interval cancers that result in poor survival rates, according to Kerlikowske.
"Breast density measures can be used to inform a woman's risk of interval cancers up to five years after breast density assessment such that a supplemental screening strategy could be implemented early to decrease the chance of diagnosis of an interval cancer," she said.
As of now, 35 U.S. states currently mandate reporting of breast density and discussion of supplemental imaging for those with dense breasts.
"Women who are accurately identified to have dense breasts and high risk of an interval cancer are more likely to have appropriate discussions of whether supplemental imaging is right for them," she said.
Kerlikowske said the researchers are now performing ongoing studies to develop risk-prediction models for interval and advanced cancers that include breast density and deep-learning measures to inform the identification of women who need supplemental imaging beyond mammography.
A cautionary tale?
An accompanying editorial in the Annals of Internal Medicine called for a cautious approach to adopting automated breast density measurement, however.
While acknowledging that the UCSF-led study offered several methodological strengths, its authors emphasized comparisons that aren't used in clinical practice, according to Dr. Joann Elmore of the David Geffen School of Medicine at the University of California, Los Angeles and Dr. Jill Wruble of the Yale School of Medicine. Women in the U.S. are advised that their breast tissue is dense if it is categorized as BI-RADS density categories C (heterogeneously dense) or D (extremely dense); the study authors focused, though, on comparing density category D with category B (scattered fibroglandular densities).
"Because three times more women receive a BI-RADS density assessment of (c) than (d), the study's focus may have limited the generalizability of its conclusions," Elmore and Wruble wrote.
While automated measurement technology is new, it remains to be determined if it offers an improvement, according to Elmore and Wruble. They noted that the breast imaging community's experience with computer-aided detection (CAD) software may serve as a cautionary tale.
"In the 20 years since the U.S. Food and Drug Administration approved CAD and its implementation became widespread -- at a cost exceeding $400 million each year -- its value has been questioned," they wrote.
For example, a 2007 study in the New England Journal of Medicine reported higher breast biopsy rates from the use of CAD without any associated improvement in detecting invasive breast cancer, while a follow-up study in 2015 concluded that CAD was associated with lower accuracy. Despite these reports, widespread use and Medicare coverage of CAD continue, according to Elmore and Wruble.
Automated density measurements do have the potential -- like CAD -- to improve reproducibility and workflow efficiency, they wrote.
"However, we are in an era of 'choosing wisely' and seeking value in healthcare," they noted. "Therefore, we must be cautious before implementing and paying for medical technology."