In a large Dutch study, using supplemental MRI screening in women with extremely dense breast tissue and normal mammograms resulted in significantly fewer interval cancers than using mammography alone.
The multicenter, randomized, controlled trial included more than 40,000 women with extremely dense breast tissue and normal results on screening mammography. Women were invited to undergo supplemental MRI or to only receive mammography screening during a two-year period. The interval cancer rate for the MRI group was cut in half, according to the research published in the New England Journal of Medicine (November 28, 2019, Vol. 381:22, pp. 2091-2102).
"This is a very important step toward proving the clinical utility of supplemental MRI screening in women with extremely dense breasts," corresponding author Carla van Gils, PhD, from the Julius Center for Health Sciences and Primary Care in Utrecht, the Netherlands told AuntMinnie.com. "This is the first time this research question has been addressed through a randomized, controlled trial, and the results are positive. If the benefits outweigh the harms, then the results pave the way from one-size-fits-all screening to a tailor-made screening approach."
MRI screening
Extremely dense breast tissue increases the risk of breast cancer fourfold and makes it harder to detect cancer using mammography alone. These patients benefit from a tailored breast screening strategy using modalities such as ultrasound or MRI.
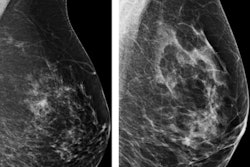
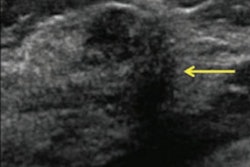
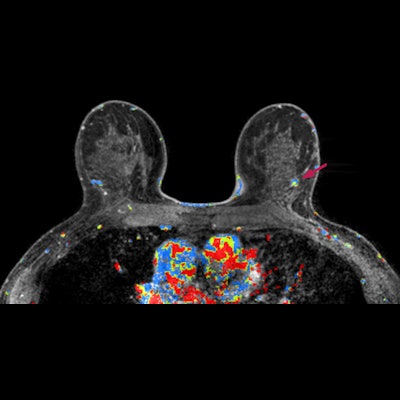
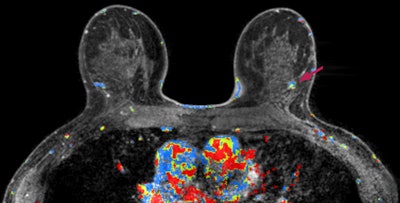 An MRI screening with a possible breast abnormality in the left breast (right side of the picture). Image courtesy of Carla van Gils, PhD.
An MRI screening with a possible breast abnormality in the left breast (right side of the picture). Image courtesy of Carla van Gils, PhD."Although supplemental imaging increases the rate of cancer detection in women with dense breasts, the question remains whether it improves health outcomes," wrote lead author Marije Bakker, PhD, also from the Julius Center for Health Sciences and Primary Care, and colleagues.
The first indication of efficacy is a reduction in the incidence of interval cancers because that means potentially symptomatic cancers would now be detected earlier. Bakker and her colleagues sought to determine just that in their study that presents the primary outcome of the first two-year screening round of the Dense Tissue and Early Breast Neoplasm Screening (DENSE) trial.
From December 2011 to November 2015, they invited 40,373 women between the ages of 50 and 75 with extremely dense breast tissue and normal results on screening mammography to either receive supplemental MRI or to receive mammography screening only. The MRI-invitation group included 8,061 women and the mammography-only group included 32,312 women.
Not all women who were invited underwent MR imaging -- only 59% accepted the invitation. For a comparison of MRI versus mammography, see the table below.
| DENSE trial supplemental MRI vs. Mammography alone | ||
| MRI | Mammography | |
| Interval cancer detection rate | 2.5 per 1,000 screens | 5.0 per 1,000 screens |
| Interval cancers | 20/8,061 | 161/32,312 |
The overall cancer detection rate -- not just interval cancers -- in the MRI group was 16.5 per 1,000 screens.
The researchers also found MRI resulted in 92% specificity, 95.2% sensitivity, and a false-positive rate of 8%. The positive predictive value was 17.4% for recall and 26.3% for biopsy.
Cancers detected in the MRI-invitation group appeared to be better differentiated and more often were hormone-receptor positive than those in the mammography-only group. At the next mammography screening, the cancer detection rate was 2.0 per 1,000 screens among the MRI participants, compared with 6.0 per 1,000 screens among the women in the mammography-only group.
"These findings indicate that MRI examination advanced the time of diagnosis," Bakker and colleagues wrote.
The strengths of the DENSE trial include the randomized design, the population-based screening cohort, the multicenter design with different centers using standardized MRI protocols from different vendors, the use of fully automated and volumetric measurements of mammographic density, and the completeness of the data collection.
A limitation is that the DENSE is not large enough to look at the effect of MRI screening on breast cancer-specific or overall mortality because that would require a much larger sample size and longer follow-up.
Future research in the two incident screening rounds will reveal the value of ongoing supplemental MRI screening versus one-time-only supplemental screening. The study authors will use a mathematical model to estimate the impact of MRI supplemental screening in the longer term as well as the effect on breast cancer mortality and the amount of overdiagnosis. They also plan to evaluate methods to reduce false positives, for example through machine learning.