Women with early-stage breast cancer who had to delay surgery due to the novel coronavirus pandemic are unlikely to experience worse survival rates, according to the findings of a study published on August 6 in the Journal of the American College of Surgeons.
The study included nearly 379,000 patients who had been treated for early-stage breast cancer in 2010 to 2016 but also delayed their initial operation by up to a year after their diagnosis. An initial delay in cancer operation did not affect the overall survival of patients, the authors found.
"We can tell our patients they can still expect an excellent prognosis from their early-stage hormone receptor-positive cancer and that their excellent prognosis is not negatively impacted by this delay they have experienced," stated senior study author Dr. Elizabeth Mittendorf, PhD, a professor of surgery at Brigham and Women's Hospital in Boston, in a press release.
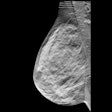
The authors used data from the National Cancer Database, one of the largest cancer registries of its kind. They focused on women with either ductal carcinoma in situ (DCIS) or small invasive tumors that hadn't spread to the lymph node -- the two groups of patients who were most likely asked to postpone cancer surgeries earlier this year.
Patients with ER-positive DCIS had a slight increase in odds of pathologic upstaging if more than 60 days passed between diagnosis and surgery, and those with ER-negative DCIS had an increased risk of upstaging if they waited more than 120 days before surgery. In either case, the increase in upstaging had no impact on the overall survival of patients.
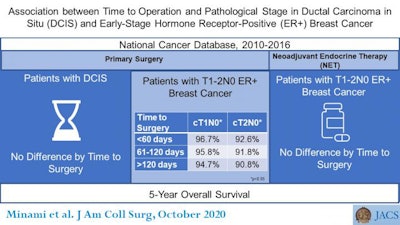 Association between time to operation and pathological stage for DCIS and ER-positive breast cancer. Image courtesy of the American College of Surgeons.
Association between time to operation and pathological stage for DCIS and ER-positive breast cancer. Image courtesy of the American College of Surgeons.As for patients with invasive early-stage breast cancer, a delay between diagnosis and operation had no significant association with pathologic upstaging. There was also no decrease in survival rates for women with estrogen-sensitive, early-stage breast cancer who were treated with neoadjuvant endocrine therapy (NET).
The authors cautioned that the patients who underwent NET in the study differ slightly from patients affected by the coronavirus pandemic. Notably, NET was not as widely used for early-stage, ER-positive outcomes in 2010-2016, and participants who underwent NET were likely older or had coexisting illnesses.
"What we can say from our findings is that despite the delay in surgical therapy, because you were on neoadjuvant endocrine therapy, we do not think that your survival will at all be impacted," stated lead study author Dr. Christina Minami, an associate surgeon at Brigham and Women's Hospital.