The benefits of digital breast tomosynthesis (DBT) may be limited for finding additional cancers in breast cancer survivors, according to a December 22 study in Radiology. While DBT led to fewer recalls, the modality didn't boost the cancer detection rate for this high-risk population.
DBT has repeatedly proved its worth as a screening tool for women in the general population, but researchers have paid less attention to its use for cancer surveillance in women with a personal history of breast cancer. The new study suggests breast cancer survivors may see more benefit from alternative screening modalities, such as MRI.
"Among breast cancer survivors, screening with digital breast tomosynthesis led to fewer false-positive results and higher specificity but did not affect cancer detection," wrote the authors, led by Dr. Manisha Bahl, director of the breast imaging fellowship program at Massachusetts General Hospital.
The authors retrospectively reviewed screening mammograms in breast cancer survivors before and after a clinic converted from digital mammography (DM) systems to DBT. With 9,019 DM exams and 22,887 DBT exams, the researchers believed the study is the largest one to date to evaluate the use of DBT for breast cancer survivors.
| DM vs. DBT in women with a personal history of breast cancer | |||
| DM | DBT | p-value | |
| Abnormal interpretation rate | 6.2% | 5.8% | 0.001 |
| Specificity | 94.7% | 95% | 0.003 |
| Overall cancer detection rate | 10.6 | 8.3 | 0.07 |
| Invasive cancer detection rate | 74% | 72% | 0.69 |
Bahl and colleagues found that DBT led to a lower abnormal image interpretation rate and higher specificity than digital mammography in this population. But the overall and invasive cancer detection rates did not differ between the two modalities.
Furthermore, one-third of the 86 interval cancers that developed in the cohort were visible on screening MRI. At the same time, physicians were less likely to refer patients to MRI after the introduction of DBT. This potentially led to a missed opportunity for early cancer detection in breast cancer survivors.
"We found that use of screening MRI was lower in the DBT than the digital mammography era, which could be due to referring physicians' increased confidence in DBT," the authors wrote.
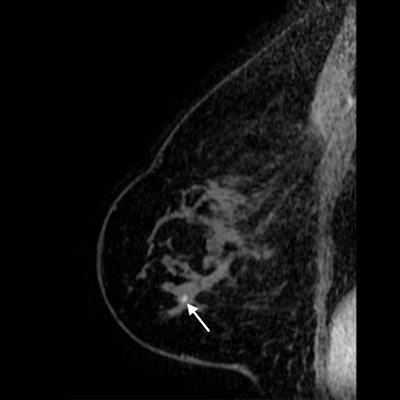 Sagittal T1-weighted fat-saturated contrast-enhanced MRI image of 71-year-old woman with history of breast cancer who presented for screening MRI. Arrow points to 4-mm focus in right breast at middle depth. MRI-guided core needle biopsy showed grade 1 invasive lobular carcinoma. All images courtesy of RSNA.
Sagittal T1-weighted fat-saturated contrast-enhanced MRI image of 71-year-old woman with history of breast cancer who presented for screening MRI. Arrow points to 4-mm focus in right breast at middle depth. MRI-guided core needle biopsy showed grade 1 invasive lobular carcinoma. All images courtesy of RSNA. Screening mammography image of same patient taken six months prior. Right mediolateral oblique tomosynthesis image was interpreted as benign, with the circle highlighting postsurgical changes. The cancer diagnosed after MRI screening was confirmed to be an interval cancer.
Screening mammography image of same patient taken six months prior. Right mediolateral oblique tomosynthesis image was interpreted as benign, with the circle highlighting postsurgical changes. The cancer diagnosed after MRI screening was confirmed to be an interval cancer.The findings led the authors to question the clinical relevance of DBT for women with a personal history of breast cancer. Although significant, the absolute reduction in the abnormal image interpretation rate was fairly small at 0.4%. Still, the higher specificity could be a benefit for women with prior cancer by reducing the number of women recommended for biopsy.
"This benefit of DBT could lessen the anxiety experienced by most breast cancer survivors upon presenting for mammography," Bahl and colleagues wrote.
The authors cautioned their study specifically excluded women screened with DBT during the two transition years to the modality. As a result, DBT's cancer detection rate could have been higher if all first exams were included.
Nevertheless, the researchers said their findings more readily support the use of MRI screening for women with a prior breast cancer diagnosis. The findings go to show that MRI continues to visualize cancers that mammography can't -- even in the DBT era.
"Given that the cancer detection rate did not significantly change after DBT integration and that one-third of interval cancers were detected at MRI, our results suggest that supplemental screening with MRI will continue to be useful in this high-risk population," the authors concluded.