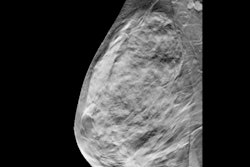
A prototype device combining 3D automated breast ultrasound (ABUS) and digital breast tomosynthesis (DBT) performed well in a feasibility study published on December 12 in European Radiology. The system identified 97% of cancers and added only about a minute to the DBT exam time.
The team created the device by modifying existing ABUS and DBT technology from Siemens Healthineers. Their custom system visualized all but one cancer case, and a breast diagnostic specialist rated the ABUS and DBT images as diagnostically useful in 85% of patient cases.
"If tomosynthesis and ABUS should become part of breast cancer screening, the combination of both techniques in one device could offer practical and logistic advantages," wrote the authors, led by Dr. Benedikt Schäfgen, an ob/gyn resident and research fellow in the breast unit at University Hospital Heidelberg in Heidelberg, Germany.
The team created their Fusion-X-US-II prototype by modifying an Acuson S2000 automated breast volume scanner (ABVS) and Mammomat Inspiration mammography system from Siemens. They described the first version of the scanner, the Fusion-X-US-I, in a 2018 European Radiology article.
The newer version improved upon the first by adapting the compression panel's size and weight to provide better patient positioning. The team also added an air cushion, which a radiologic technologist could inflate for improved contact between the breast surface and ultrasound probe.
The team tested the new and improved FUSION-X-US-II system in a prospective cohort study of 101 women recommended for diagnostic DBT imaging at the Heidelberg breast unit in 2019.
All patients first underwent a standard workup with both 2D mammography, handheld ultrasound, and DBT. Then, they underwent DBT followed by ABUS with the Fusion-X-US-II prototype. Total exam time with the prototype ranged from one minute and 30 seconds to just over two minutes.
The prototype achieved a sensitivity of 97% and specificity of 60%. The radiologist reading the prototype images correctly identified 33 out of the 34 malignant lesions -- 26 visible on both DBT and ABUS, six only visible on DBT, and one only visible on ABUS.
The one cancer missed by the prototype was localized close to the thoracic wall in a woman with macromastia. It was identified on handheld ultrasound in the standard workup but not on DBT.
The addition of ABUS helped the reading radiologist to better visualize cancers seen on DBT. With ABUS images, the radiologist correctly upgraded three cases of breast cancer -- two from BI-RADS 4B to 5 and one from BI-RADS 4A to 4B. In addition, ABUS identified invasive lobular carcinoma not seen on DBT.
"In this case, the combined analysis of ABUS and tomosynthesis showed a clear advantage over tomosynthesis alone," the authors wrote. "In the standard diagnostic workup, this carcinoma presented as a palpable lesion with a sonographic correlate in [handheld ultrasound] but no mammographic correlate."
Overall, the prototype showed improvements over the first version and achieved greater surface area coverage (80% versus 66%). The authors also agreed Fusion-X-US-II proved itself to be feasible and time-efficient.
That said, there's still room for improvement. Notably, one-third of the patients initially eligible for the study could not complete ABUS due to software errors and hardware problems -- most often an inability to start or finish the scan and failure to save or transmit ABUS data.
The prototype also struggled with ABUS image quality. The reading radiologist rated most ABUS scans as having well-distinguishable tissue structures but a lower quality than handheld ultrasound. A total of 7% of lesions were also only partly visualized on ABUS and 11% were classified as BI-RADS 0 due to low image quality.
The team chalked up the image quality issues to the transducer, noting they will need to adapt a high-end transducer in order to improve images acquired with the prototype. Fortunately, they're already working on that for version 3 of Fusion-X-US.
"A large part of the missing breast area is due to the blind gap of approximately 1 cm towards the pectoralis muscle caused by the housing of the ABUS device," the group wrote. "To reduce this shortcoming, a dedicated ultrasound transducer with optimized housing and position of active ultrasound elements will be tested in future prototypes."