It's time to consider risk-adapted breast cancer screening, said Jack Cuzick, PhD, the co-creator of the Tyrer-Cuzick breast cancer risk assessment model, on Friday at the Society of Breast Imaging/American College of Radiology Breast Imaging Symposium.
 Jack Cuzick, PhD.
Jack Cuzick, PhD.The strongest risk factors currently identified for breast cancer are breast density and the polygenic risk score, based on single-nucleotide polymorphisms (SNPs), according to Cuzick. These variables were added in the current version (8) of the Tyrer-Cuzick (IBIS) Model, which was released in 2017.
"There's already adequate information out there to begin to think about risk-adaptive screening," said Cuzick of Queen Mary University of London. "We shouldn't just be screening everybody the same way. What we need to do is develop a structure and experience in how to collect this data effectively."
Under a risk-adapted screening strategy, high-risk women would receive more intensive screening -- such as MRI -- and potentially the use of preventive therapy, according to Cuzick. Meanwhile, low-risk women "probably" need less or even no screening due to potential side effects such as radiation exposure and harms such as false positives, he said.
"Where benefits are minimal, side effects are more important," he added.
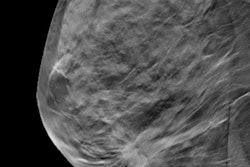
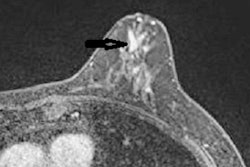
Breast density is one of the most important known risk factors. Density measurements are "strongly correlated" with age and body mass index (BMI), Cuzick said.
"It [density] goes down with age, particularly after the menopausal period, and goes down with lower BMI," he noted.
In a 2015 IBIS study led by Cuzick that was published in Lancet Oncology, the hormonal therapy drug tamoxifen's effects in preventing breast cancer were observed in women with a density reduction of at least 10% at 12 to 18 months.
Cuzick also highlighted the importance of polygenic risk scores, which are created from panels of SNPs and show how a person's risk compares with those with a different genetic constitution. Over 300 SNPs have been found, each carrying a small risk (± 5%-10%). However, panels of dozens or even hundreds of SNPs can be useful in measuring risk in patients, according to Cuzick.
For example, a 2020 study in JAMA Network Open found that an 86-single-nucleotide variation score was useful in stratifying breast cancer risk in carriers of breast cancer susceptibility genes such as CHEK2 and BRCA1, he said.
Efforts to develop risk-adapted screening strategies should probably be undertaken by screening facilities, Cuzick added. But the public should also be involved in these decisions.
"We have to make sure we involve the public in these things, particularly for low-risk women who have been trained to think that mammograms are good for them," he said.