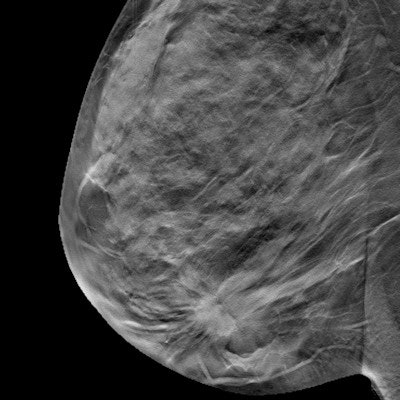
Women with dense breast tissue who received supplemental whole-breast ultrasound with their digital breast tomosynthesis (DBT) screening exams had a lower rate of abnormal interpretations in a study presented at the 2021 American Roentgen Ray Society (ARRS) meeting.
The combination of screening with DBT and whole-breast ultrasound cut the number of abnormal findings in half and could result in lower recall rates compared to screening with DBT alone, according to researchers from Yale University and the University of Massachusetts.
"This is likely due to the improved confidence by the radiologist in interpreting DBT in conjunction with whole-breast ultrasound, and the ability to generate a more comprehensive assessment by combining findings on both exams," said Cameron Thomson, an undergraduate researcher from the University of Massachusetts.
Whole-breast ultrasound is a relatively low-cost, noninvasive option for screening, and it has also been shown to detect an additional 1.1 to 4.6 cancers per 1,000 patients. However, it has been criticized for having a high false-positive rate, which increases screening recall rates.
DBT, meanwhile, has been shown to decrease the mammography screening recall rate and yields more information than conventional 2D mammography. The University of Massachusetts has been performing whole-breast ultrasound since 2009 and has been using DBT for screening since 2011.
To examine how well the technologies worked together, Thomson et al examined 12,649 DBT screening exams performed between January 2019 and December 2019. They also included all women with dense breast tissue who received whole-breast ultrasound during the same period.
The screenings were of female patients with heterogeneously (11,314) or extremely (1,335) dense breasts. About one-third of these women (4,115) underwent DBT only and the other two-thirds (8,534) underwent concurrent DBT and whole-breast ultrasound.
Screening whole-breast ultrasound was performed by trained technologists and interpreted online by radiologists on-site to check abnormal findings, which were represented by BI-RADS classification. DBT studies classified as BI-RADS 0, 3, 4, and 5 were considered to be abnormal, while BI-RADS 1 and 2 were classified as normal. There were no BI-RADS 0 studies among the whole-breast ultrasound, so abnormal studies were defined as 3, 4, and 5.
The researchers found that the addition of whole-breast ultrasound to DBT reduced the overall rate of abnormal findings from 14% to 6.7% (p < 0.00001); this represents a twofold reduction in the abnormal interpretation rate for women with dense breast tissue. This reduction occurred even as ultrasound found an additional 2.9% of suspicious findings that had been missed with DBT alone.
| Abnormality rate of DBT + whole-breast US for breast screening | |||
| Whole-breast US only | DBT only | DBT plus whole-breast ultrasound | |
| Rate of abnormal findings | 4.2% | 14% | 6.7% |
The team said findings like these are important, as women with dense breast tissue can benefit from additional cancer detection without adverse false positives.
"These findings are important as this potentially permits women with dense breast tissue the opportunity to benefit from additional cancer detection without the fear of increased adverse, abnormal interpretation rates when opting for supplemental screening with whole-breast ultrasound," Thomson said.




















