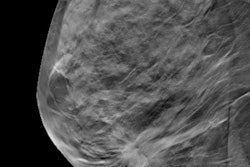
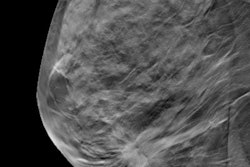
A new study published August 30 in JAMA Internal Medicine is blaming increased adoption of digital breast tomosynthesis (DBT) for rising costs of screening mammography among privately insured women in the U.S.
A team led by Dr. Ilana Richman from Yale University found that while the cost of a 2D mammogram remained stable during the study period of 2013 and 2019, the average cost of DBT exams (also known as 3D mammography) grew, as did overall spending on mammography by women with private insurance.
"This study gives us some sense of the magnitude of how DBT adoption may add to screening costs," Richman told AuntMinnie.com. "We also found that DBT does not save money, at least in the short term, which may be somewhat surprising given that many studies have shown DBT may reduce the need for follow-up testing."
DBT has shown promise in previous studies of being superior to 2D mammography for breast cancer screening. Research suggests that while DBT may cost more, it may generate downstream savings by reducing the number of women called back for additional imaging.
In the current study, the researchers wanted to characterize changes in the costs of breast cancer screening at both the patient and provider levels as DBT was being adopted.
The team looked at data from 8,432,037 women between 2013 and 2019 who underwent 15,669,701 screening mammograms. The women were 40 to 64 years of age.
Richman et al found that the proportion of mammograms billed with DBT rose from 13% in early 2015 to 70% in early 2019, evidence of the rapid adoption of 3D mammography in the U.S.
But annual screening expenditures for privately insured women ages 40 to 64 years also rose with growing DBT adoption, increasing from about $3.9 billion in 2013 to $5.2 billion in 2019, the team found. If DBT had been used for 100% of those exams rather than just 70%, the cost would have been even higher.
"Assuming 2019 costs, if DBT were used for screening all women in this population, the total cost would be $5.4 billion per year, compared with $4.2 billion for screening with 2D, a difference of $1.1 billion," the study authors wrote.
| Screening mammography costs | ||
| 2013 | 2019 | |
| Total cost of breast screening for privately insured women | $3.9 billion | $5.2 billion |
| Average cost of screening mammogram | $239.80 | $295.60 |
| Average cost of 2D mammogram | $239.80 | $238.80 |
| Average cost of DBT mammogram | $280.70 (in 2015) | $315.60 |
| Average cost of subsequent testing per screening exam | $75.30 | $99.30 |
| Average cost of screening episode | $316.40 | $396.50 |
The cost of subsequent testing meanwhile remained stable, only increasing from 12% in early 2013 to 13% in early 2019.
The researchers also found the average cost of a DBT exam was higher than that of 2D mammography at every time point and rose over time, from $280.70 in 2015 to $315.60 in 2019.
While higher screening costs are acceptable if they result in sufficient improvements in health or quality of life, DBT may be associated with "small gains" in quality of life and is generally not cost-effective, they wrote.
Richman said the team is working on related projects about how costs and insurance coverage for DBT may influence women's screening choices.
Advocates for breast screening have called into question the methodology used to develop the cost estimates. DBT codes for reimbursement were introduced for Medicare patients early in 2015, but private insurers did not begin paying for the exam until years later, according to Dr. Stamatia Destounis, chief of the American College of Radiology's breast imaging committee.
"Does that falsely then reduce the costs earlier on during this review's timeline, as patients were likely paying out of pocket for the DBT examination?" Destounis said.
Destounis told AuntMinnie.com the study mixes supplemental screening populations and does not ask if the cancer detection rate increased during the time frame of DBT implementation.
"So, at this point, it is unclear what the value of this study is at all in determining cost-effectiveness of DBT," she said. "We look forward to further research on the subject of DBT cost-effectiveness including reduced recall rates, increasing cancer detection, and increasing patient satisfaction."