Digital breast tomosynthesis (DBT) has shown itself to be a valid, beneficial breast imaging technology over a decade after it first became commercially available, according to research presented Sunday at the RSNA 2021 annual meeting.
In her presentation, Dr. Liane Philpotts from Yale University discussed her team's findings from an eight-year study that showed DBT screening metrics have held steady with favorable recall rate, cancer detection rate, and false-negative rates for women with dense and nondense breasts.
"We feel that the maintained benefits of DBT support use of this technology for screening," Philpotts said.
DBT first became commercially available in the U.S. in 2011, with Yale offering such screening that same year. While studies over the last 10 years have suggested this screening method is superior to conventional mammography in terms of recall and cancer detection rates, researchers acknowledge that long-term studies are needed for newer technologies.
Philpotts and colleagues wanted to show DBT's promise through a 10-year study. For the first eight years of the study, the team also performed screenings in their mobile van that also had a 2D mammography unit.
The team looked at recall rates, cancer detection rates, positive predictive value of recall, and false-negative rates.
A total of 237,108 DBT mammograms were performed. Of these, 150,070 were of nondense breasts while 87,038 were dense.
| Comparison of average aggregate DBT (10 years) and mammography (8.5 years) screenings | ||
| 2D mammography (8,844 cases) | DBT (237,108 cases) | |
| Recall rate | 13.3% | 7.2% |
| Cancer detection rate | 4.5 per 1,000 | 5.5 per 1,000 |
| Positive predictive value | 3.4% | 7.6% |
The recall rate for DBT ranged between 6.6% and 8.8% over the 10 years, peaking at the second year.
Greater fluctuations were seen with DBT's positive predictive value, with a range between 5.6% and 8.8%. The false-negative rate for the first nine years averaged 0.6 per 1,000 exams.
The average recall rate was higher for women with dense breasts at 7.9%, compared with women with nondense breasts at 6.8% (p < 0.001). Women with dense breasts also had a lower cancer detection rate at 5.1 per 1,000 compared to the 5.8 per 1,000 detected in women with nondense breasts (p = 0.02), as well as a lower positive predictive value (6.4%) than in women with nondense breasts (8.5%, p < 0.001).
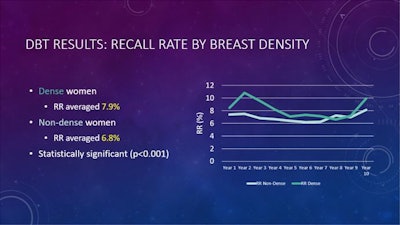 The recall rate for women with dense breasts was significantly higher than that of women with nondense breasts on DBT readings. Dr. Liane Philpotts from Yale University said this supports the need for supplemental screening for women with dense breasts. Image courtesy of Dr. Liane Philpotts.
The recall rate for women with dense breasts was significantly higher than that of women with nondense breasts on DBT readings. Dr. Liane Philpotts from Yale University said this supports the need for supplemental screening for women with dense breasts. Image courtesy of Dr. Liane Philpotts.Philpotts said the higher incidence of cancers detected in the dense breast group supports supplemental screening for these women.
"It's certainly harder to find those cancers," she said. "We do a lot of supplemental screening where I practice in Connecticut. A lot of these women with denser tissue have had cancers detected with supplemental screening. As good as DBT is, it doesn't find all the cancers, so I think the results are reasonable there."
She also explained that DBT recall rates in the U.S. may be higher than in some European studies due to differences in screening intervals. However, Philpotts added that reducing recall rates is "absolutely key."
"I feel like the biggest benefit for DBT is reducing the recall and false-positive rates," she said. "I think everyone has to assess their own differences with DBT and 2D [mammography]."