Younger, premenopausal women's estimated breast cancer risk is influenced by adding mammographic density to the Tyrer-Cuzick risk model, according to research shared at the recent RSNA meeting.
Dr. Stamatia Destounis of Elizabeth Wende Breast Care in Rochester, NY, discussed results she and her team found by adding volumetric breast density and BI-RADS to the version 8 Tyrer-Cuzick model's list of factors.
Breast density is linked to higher cancer risk, due not only to its strength as a risk factor but also its prevalence among women. It is now included in several risk assessment models and can improve risk stratification, the investigators wrote. The Tyrer-Cuzick model is one of the most widely used for assessing breast cancer risk. While the latest version includes breast density as a risk factor, it does not provide guidance for whether to use volumetric breast density percentage or BI-RADS for measuring breast density, according to Destounis.
She and her team sought to investigate the impact of mammographic density measures on clinically actionable breast cancer risk estimates reported by the Tyrer-Cuzick model. The group conducted a study that included data from 59,257 women who underwent risk assessment using Tyrer-Cuzick version 7 at the time of screening between July 2019 and January 2020. The investigators also considered volumetric breast density percentage and BI-RADS using version 8 of the Tyrer-Cuzick model. Study participants had an average age of 59 years, an average body mass index of 29.9, and an average volumetric breast density of 8.4%. Postmenopausal women accounted for most of the study group (67.9%).
Destounis and colleagues found that compared with the 8.3% of women classified as high-risk using the version 7 model with no density input, there was a significantly higher proportion of high-risk women when using version 8 with volumetric breast density (11.4%). However, they also found a significantly lower proportion of high-risk women when using version 8 with BI-RADS (6.9%).
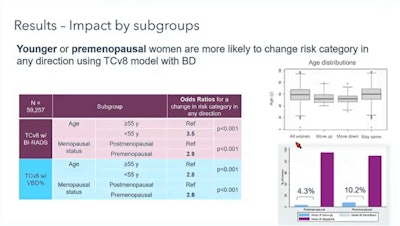 Research presented at RSNA shows that adding breast density to version 8 of the Tyrer-Cuzick model impacts breast cancer risk for younger, premenopausal women. The above chart shows how odds ratios are impacted with the additions of volumetric breast density and BI-RADS to version 8 compared with version 7 of the model, which had no breast density inputs. Image courtesy of Dr. Stamatia Destounis.
Research presented at RSNA shows that adding breast density to version 8 of the Tyrer-Cuzick model impacts breast cancer risk for younger, premenopausal women. The above chart shows how odds ratios are impacted with the additions of volumetric breast density and BI-RADS to version 8 compared with version 7 of the model, which had no breast density inputs. Image courtesy of Dr. Stamatia Destounis.Women under the age of 55 had an odds ratio of 2.8 when using volumetric breast density and 3.5 using BI-RADS (p < 0.001) when considering a change in risk category in either direction by including density. Premenopausal women had an odds ratio of 2.6 when using volumetric breast density and 2.9 using BI-RADS.
Of the 896 (1.5%) women who became low risk by adding density to the risk assessment tool using volumetric breast density, the researchers found 144 with a family history of a first degree relative with breast cancer under the age 45. Of women at low or intermediate risk using version 8, 36% had dense breasts.
"Clinics wanting to establish high-risk screening programs should understand that different mammographic density measures incorporated into risk models can differentially impact patient management," Destounis and colleagues concluded.