Breast imagers have and continue to face challenges posed by the COVID-19 pandemic, said Dr. Debra Ikeda in a May 17 at the Society of Breast Imaging/American College of Radiology symposium in Savannah, GA.
In her talk, Ikeda from Stanford University in California talked about the myriad ways the pandemic has impacted breast radiologists, from mental wellness to financial security and more. She also had words of encouragement.
"In these challenging times, be compassionate. There can be suffering, but you can have compassion," Ikeda said. "Show appreciation for each other. You are doing a good job."
When the pandemic first hit the U.S. in spring 2020, it hit radiology hard as lockdowns kept many patients away from hospitals and imaging centers. Imaging volumes fell dramatically and remained below pre-pandemic levels even as facilities began reopening in late summer.
In California, where Ikeda works, 77% of breast imaging facilities reduced imaging services and 13% shut down completely, according to a survey Ikeda worked on that was published in March 2021.
"We didn't know," Ikeda said about COVID-19's symptoms and transmission. "You didn't know how it was transmitted. Many regions fell under government restrictions."
After reopening, practices adjusted how they imaged patients. Studies reported increased use of personal protective equipment (PPE) such as masks and gowns, as well as increased use of telehealth equipment in physician homes. For the latter, a 2021 study reported that it cost practices an average of $79,000 for first-year costs and $18,000 for annual ongoing costs.
For radiologists, students, and other staff, however, the challenges of the pandemic went beyond practice numbers.
Effects on mental wellbeing
With the uncertainties surrounding imaging during the pandemic, radiologists also reported mental struggles. A 2021 study Ikeda cited in her presentation reported that 68% of breast radiologists suffered from anxiety. About 41% of survey respondents reported experiencing sadness, while 36% reported having sleeping problems. Anger and depression were also reported among radiologists.
In the same study, the authors wrote that women and younger radiologists had higher psychological distress scores. Also, 37% of survey respondents who had children reported that childcare needs adversely affected their jobs, and they also reported higher distress scores.
"Because of gender disparities, there is a need to work proactively for support strategies for young women staff and faculty," Ikeda said.
Ikeda also noted the challenges faced by technologists during the early months of the pandemic, calling them the first line of imaging.
"They have a high-risk role," Ikeda said. "They have to modify their positioning and cleaning regiments. The pandemic continued to evolve, so we had different regiments at different times."
She added that going off current literature, technologists should be included in decision-making for practices.
Financial challenges
Due to the temporary stoppage of nonemergency imaging services, pay for radiologists also generally decreased. A 2021 survey study in Journal of Breast Imaging by Chalfant et al reported that 87% of imaging facilities reported negative financial impacts on breast imaging physicians.
This included decreases or elimination of bonuses, productivity-based pay, and salary or hourly rate, among others. Required use of vacation or paid time off was also reported by facilities in the study.
Effects on education
The pandemic also impacted education. Many radiology trainees could not gain clinical experience due to limitations on who could work in person at practices. Students were mostly limited to virtual learning.
Ikeda co-authored a survey study published in 2021 in Journal of Breast Imaging that found that while 99% of students were not allowed on service during the pandemic's peak in spring 2020, 58% reported not being allowed on service after curve flattening. Meanwhile, 88% of residents and 71% of fellows reported fewer days per week on clinical service.
About 10% of respondents reported that future employment of their program's fellows was negatively impacted by the pandemic. These included changes in starting dates, no job opportunity, loss of a job offer, and decrease in salary and time off.
For educators, previous studies reported that it's more difficult to create lesson plans for online-only learning environments and that there is a risk of social isolation. Hybrid learning environments have been proposed to bridge these gaps.
"Education was strongly affected and there are several gaps," Ikeda said. "Could you imagine being a first-year resident and trying to read a mammogram from home? That's very difficult."
Vaccine-related lymphadenopathy
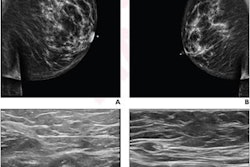
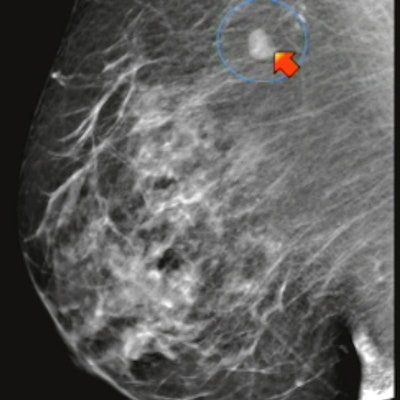
Soon after the COVID vaccines began rolling out, patients and radiologists noticed one side effect that presented on mammography. Axillary lymphadenopathy presented as a swollen lump, though in most cases, the lumps were benign and needed time to recede.
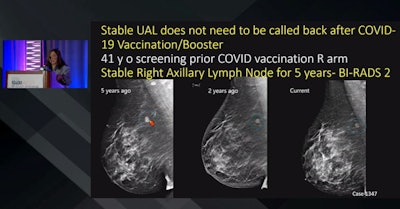 Radiologists are more experienced with axillary lymphadenopathy related to COVID-19 vaccines, according to a presentation given by Dr. Debra Ikeda (inset) from Stanford University. Here, images of a 41-year-old patient show a stable right axillary lymph node before vaccine administration, meaning the patient doesn't need to be called back in for an unnecessary biopsy. Ikeda also talked about the many challenges breast imagers have faced during the COVID-19 pandemic.
Radiologists are more experienced with axillary lymphadenopathy related to COVID-19 vaccines, according to a presentation given by Dr. Debra Ikeda (inset) from Stanford University. Here, images of a 41-year-old patient show a stable right axillary lymph node before vaccine administration, meaning the patient doesn't need to be called back in for an unnecessary biopsy. Ikeda also talked about the many challenges breast imagers have faced during the COVID-19 pandemic.Early recommendations included delaying mammograms anywhere between four weeks and 12 weeks for vaccine-related symptoms such as lymphadenopathy to subside.
However, the SBI in March came out with updated recommendations saying women should no longer delay screening mammograms around vaccinations. These came after several position statements, opinion pieces, and single-institution retrospective studies over the past year.
"Radiologists are now more familiar and experienced with post-vaccine lymphadenopathy," Ikeda said. "When they first developed these guidelines, they wanted to reduce unnecessary workups. But now that everyone knows that it's image-detected, clinically apparent, and can be earlier and last longer than initially expected."
Ikeda co-authored data being presented at the symposium showing that about 10% of over 3,000 patients had ipsilateral axillary lymphadenopathy following vaccination and that no additional cancers were found on clinical or ultrasound follow-up.