Mammograms performed with women compressing their own breasts have comparable image quality and with significantly stronger breast compression, suggests an Italian study published July 22 in European Radiology.
Researchers led by Dr. Valentina Iotti from IRCCS of Reggio Emilia also found that self-compression did not seem to have any impact on participation with follow-up mammography.
"Our sample could not identify any difference in compliance to follow-up visits because it was close to 100% in both arms," Iotti and colleagues wrote.
Breast compression is needed to reduce radiation scattering and thus ensure high-quality mammograms, but it also causes pain and discomfort for women. Previous research suggests that 25% to 46% of women cite pain as a reason for not attending follow-up breast cancer screening.
Research has also shown that better communication between mammography staff and women can help ease the breast compression process. Self-compression tools have also been developed. While these tools help with patient satisfaction, little evidence exists that they lead to increased future participation.
Iotti et al wanted to find out whether self-compression could reduce the average glandular dose through better compression and whether it could lead to higher compliance with follow-up mammography compared with standard compression led by radiologists and radiographers. They hypothesized that self-compression could lead to less unpleasant memories of pain and discomfort when going for follow-up mammograms.
The researchers looked at prospective data from 495 women with an average age of 57. The women were randomly placed in either a self-compression arm (n = 245) or compression arms led by radiologists and radiographers (n = 250).
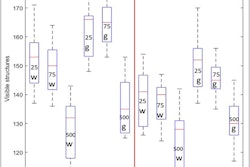
Compression force was measured in decanewtons (daN), while image quality was measured on a scale of 0 to 35, with higher numbers indicating better image quality.
| Comparison of self-compression and conventional compression during mammography | |||
| Conventional compression | Self-compression | p-values | |
| Compression force | 102.5 daN | 114.5 daN | p < 0.001 |
| Compression thickness | 48.008 mm | 46.339 mm | p = 0.14 |
| Image quality (radiologists) | 29.8 | 30 | p = 0.90 |
| Image quality (radiographers) | 0.63 | 0.65 | 0.32 |
| Radiation dosage | 1.93 mGy | 1.90 mGy | 0.47 |
| Percent reporting moderate/severe discomfort | 9.6% | 7.8% | 0.77 |
| Median pain scores | 4 | 4 | 0.55 |
The researchers also found a 1.7-mm reduction in thickness in the self-compression arm, as well as no effect on subsequent mammography (p = 0.47).
"Our sample could not identify any difference in compliance to follow-up visits because it was close to 100% in both arms," they wrote.
While the conventional arm saw a median execution time of 10 minutes, the self-compression arm showed nine minutes, six seconds of execution (p < 0.001).
The team noted that the nonsignificant decrease in average radiation dose per view was counterbalanced by a slight nonsignificant increase in additional views due to incorrect positioning.
The study authors also found no differences in the memory of the pain and discomfort experienced during the study mammogram collected just before performing the subsequent mammogram. They suggested that this means self-compression isn't likely to increase or discourage participation in follow-up mammograms.
However, they also saw an inverse association between pain and discomfort and compression, suggesting that women who better tolerate pain reach higher compression force.
"Interestingly... this association was the opposite in the conventional arm. Women who received higher compression remembered a higher discomfort one year later, but in the self-compression arm, this association disappeared," Iotti et al wrote. "This finding suggests that at least some of the unpleasant memories given by compression can be redeemed by self-compression."