Digital breast tomosynthesis (DBT)-guided biopsy can help reduce patient discomfort and radiation exposure when it comes to suspicious breast calcifications, a study published September 14 in the American Journal of Roentgenology found.
Researchers led by Dr. Derek Nguyen from Johns Hopkins Medicine compared DBT-guided biopsy with conventional stereotactic-guided digital mammography biopsy and found that clinical outcomes were not affected, making DBT a potential alternative.
"DBT-guided procedures were faster than stereotactic-guided biopsies which would reduce patient discomfort during the biopsy," corresponding author Dr. Emily Ambinder from Johns Hopkins told AuntMinnie.com. "We know that these procedures are not comfortable for patients, and we are excited about the ability to do them quicker without affecting outcomes."
DBT continues to grow in use in breast care practices across the world as new research highlights its advantages over digital mammography. Previous research has shown that DBT-guided biopsy improves targeting and sampling of noncalcified lesions such as asymmetries, masses, and architectural distortion.
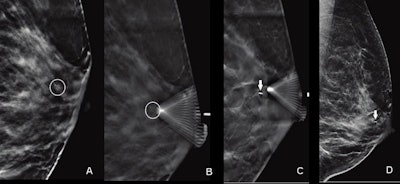 Images of a 55-year-old woman show suspicious calcifications that were recommended for biopsy. Calcifications spanned 0.6 cm in the retroareolar left breast. On the day of the procedure, the radiologist performed a DBT-guided biopsy. (A) Scout image obtained for targeting purposes demonstrates grouped amorphous calcifications (circle). (B) Prefire image obtained to confirm needle position shows tip of biopsy device adjacent to targeted calcifications (circle). (C) Postsampling image documents biopsy clip deployment (arrow). D. Postprocedure synthetic 2D diagnostic mammogram mediolateral view shows biopsy clip in appropriate position (arrow). Biopsy result was invasive ductal carcinoma. Images courtesy of ARRS.
Images of a 55-year-old woman show suspicious calcifications that were recommended for biopsy. Calcifications spanned 0.6 cm in the retroareolar left breast. On the day of the procedure, the radiologist performed a DBT-guided biopsy. (A) Scout image obtained for targeting purposes demonstrates grouped amorphous calcifications (circle). (B) Prefire image obtained to confirm needle position shows tip of biopsy device adjacent to targeted calcifications (circle). (C) Postsampling image documents biopsy clip deployment (arrow). D. Postprocedure synthetic 2D diagnostic mammogram mediolateral view shows biopsy clip in appropriate position (arrow). Biopsy result was invasive ductal carcinoma. Images courtesy of ARRS.Suspicious calcifications are "the most common" imaging finding tied to ductal carcinoma in situ (DCIS) and have a broad positive predictive value for malignancy, researchers noted. Digital mammography is typically used to guide biopsy for these calcifications, which uses multiple exposures to better target the area of interest in 3D.
However, the researchers pointed out a lack of data comparing DBT with mammography-guided biopsy when it comes to specifically sampling calcifications. Nguyen et al wanted to add to the literature, comparing the performance and outcomes of both modalities for suspicious breast calcifications.
They looked at retrospective data from 1,310 women with an average age of 58. The women underwent a total of 1,354 biopsies performed at a single institution between 2017 and 2021. The decision to use mammography-guided or DBT-guided biopsy was at the discretion of the performing radiologist. Thus, 348 of the total biopsies were performed with mammography guidance while the remaining 1,006 were guided by DBT.
| Mammography vs. DBT-guided biopsy for suspicious breast calcifications | |||
| Mammography | DBT | p-value | |
| Average procedure time (minutes) | 24.7 | 14.9 | < 0.001 |
| Average number of exposures | 9.1 | 4.1 | < 0.001 |
The researchers found no significant differences between both biopsy techniques in malignancy rate on initial biopsy, high-risk lesion upgrade rate, or final malignancy rate. They also found no significant differences between either guidance technique when accounting for patient age, breast density, calcification morphology, and calcification distribution.
The study authors wrote that their findings support the use of DBT guidance for biopsy of suspicious calcifications. They added that while the amount of radiation exposure from DBT is not significantly different from that of mammography, decreasing the total number of exposures for patients can lead to less overall radiation exposure.
Ambinder said that by using DBT to localize calcifications, the radiologist does not need to triangulate on the stereotactic images, which can be time-consuming.
"Radiologists who have access to DBT-guided biopsy can use this information to shift their practice to using this technology for biopsy of calcifications," she added.
She also told AuntMinnie.com that the team hopes to work on larger multisite prospective studies related to DBT-guided biopsies.