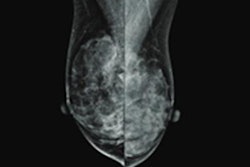
Active surveillance with mammography is the go-to choice for most women with low-risk ductal carcinoma in situ (DCIS), suggest Dutch findings published August 4 in the European Journal of Cancer.
Researchers led by Renée Schmitz, MD, from the Netherlands Cancer Institute in Amsterdam found that 76% of women surveyed "strongly" preferred surveillance over the 24% who preferred conventional treatment, with the most cited reason for the former being that treatment is "not [yet] necessary."
"Their preferences highlight the necessity to establish safety of active surveillance for low-risk DCIS," Schmitz and co-authors wrote.
While only a small number of DCIS cases progress to invasive breast cancer, European guidelines recommend surgery. However, active surveillance has been proposed in recent years as an alternative method, with proponents saying this avoids overtreatment in women with DCIS deemed to be low risk.
Schmitz and colleagues sought to describe women's preferences for choosing between active surveillance and conventional treatment, including what factors go into their choices. It used data from the nonrandomized data from the LORD trial tests. This trial began in 2015 as a randomized controlled study of noninferiority of active surveillance compared with conventional treatment. Due to slow recruitment, in 2020 the trial was converted into a nonrandomized patient preference endeavor.
Schmitz et al included data from baseline questionnaires from 377 women. They found that of the total, 288 reported surveillance as their preferred trial arm, while 89 chose conventional treatment.
Of the women who chose conventional treatment, 51% reported cancer worry and 29% reported achieving certainty as the top reasons for opting for this choice. Top reasons for women choosing active surveillance included treatment being not yet or not always necessary (59%), trust in follow-up safety (39%), and avoiding treatment side effects (30%).
Women who chose active surveillance were more likely to not have a higher level of education (odds ratio [OR], 0.49, with 1 as reference) compared with women who chose treatment. Also, women who chose surveillance more often reported shared decision-making with their oncologist when it came to determining the best strategy (OR, 2.55).
These results "provide unique insights in real-time" on treatment preferences by patients, the authors noted. For future studies, the potential impact of these preferences could be measured on the overall health, healthcare use, and quality of life for patients.
"The evident patient preference for active surveillance in the LORD-trial highlights the need for evidence on whether active surveillance for low-risk DCIS is indeed safe, and thus the importance of DCIS treatment de-escalation trials," they concluded. "Anticipating on the trial results, novel decision aids should be developed to aid patients and clinicians to make informed decisions about the management of low-risk DCIS."
The full study can be found here.