Surveillance screening via digital breast tomosynthesis (DBT) immediately after breast cancer treatment is effective, a study published on December 20 in the American Journal of Roentgenology reported.
Researchers led by Dan Do from Massachusetts General Hospital reported that while the abnormal interpretation rate was higher during the year after diagnosis compared to subsequent years, it remained at less than 10% in all years of their six-year study.
“The results support the study institution’s protocol for patients with a prior breast cancer diagnosis of returning immediately to screening mammography with DBT and can be used to inform surveillance mammography guidelines for this high-risk patient population,” Do and co-authors wrote.
Surveillance mammography is employed after breast cancer treatment. However, there is a lack of standardization in surveillance protocols, with some practices recommending diagnostic mammography for a certain number of years or indefinitely. Others, meanwhile, recommend returning immediately to screening.
The Do team evaluated performance metrics from screening DBT in women who resume screening mammography immediately after breast cancer treatment, based on the number of years since the breast cancer diagnosis. It included retrospective data from DBT exams performed between 2013 and 2019.
In total, the researchers included data from 8,090 women with an average age of 65 years who had a prior breast cancer diagnosis. This also included 30,812 screening DBT exams. They found that screening DBT showed high cancer detection rate, low abnormal interpretation rate, and high specificity.
| Surveillance screening DBT following breast cancer treatment over six-year period |
|
|---|---|
| Cancer detection rate (per 1,000 exams) |
8.6 |
| Abnormal interpretation rate |
5.7% |
| Positive predictive value |
5.1% |
| Sensitivity |
80.3% |
| Specificity |
95.1% |
| False-negative rate (per 1,000 exams) |
2.1 |
The team also reported that the cancer detection rate demonstrated a significant independent positive association with years since breast cancer diagnosis. This included an adjusted odds ratio (OR) of 1.03 for two to three years after diagnosis (4.9 per 1,000 exams). The highest rate was between eight and nine years after diagnosis (11.2 per 1,000 exams).
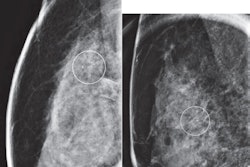
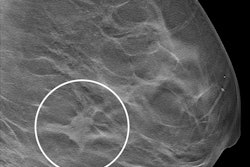
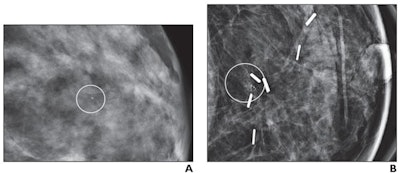 (A) Mammographic magnification view shows grouped calcifications in the left breast (circle). Stereotactic biopsy yielded grade 2 DCIS. Patient underwent a lumpectomy with tumor-negative surgical margins and radiation therapy. (B) Mammographic magnification view obtained four years after diagnosis shows new calcifications at the surgical site (circle). Stereotactic biopsy was performed, which revealed recurrent grade 2 DCIS. The patient then underwent a mastectomy. Image courtesy of the ARRS.
(A) Mammographic magnification view shows grouped calcifications in the left breast (circle). Stereotactic biopsy yielded grade 2 DCIS. Patient underwent a lumpectomy with tumor-negative surgical margins and radiation therapy. (B) Mammographic magnification view obtained four years after diagnosis shows new calcifications at the surgical site (circle). Stereotactic biopsy was performed, which revealed recurrent grade 2 DCIS. The patient then underwent a mastectomy. Image courtesy of the ARRS.
The abnormal interpretation rate meanwhile had a significant independent negative association with years since breast cancer diagnosis with an adjusted OR of 0.99 (p = .01). This was highest within one year after diagnosis (7.5%) and lowest between five and six years after diagnosis (5%).
The study authors highlighted that the abnormal interpretation rate in their study falls into an acceptable range. They added that the results support the team’s approach to mammographic surveillance with DBT.
The full study can be found here.